 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 24(1); 2022 > Article |
|
Abstract
Objective
Aneurysmal subarachnoid hemorrhage (aSAH) has a high mortality rate, and hemorrhage amounts and perioperative rebleeding importantly determines prognosis. However, despite adequate treatment, prognosis is poor in many ruptured aneurysm cases. In this study, we identified and evaluated factors related to perioperative rebleeding in patients with aSAH.
Methods
The medical and surgical records of 166 patients that underwent endovascular embolization for a ruptured cerebral aneurysm at a single institution from 2014 to 2016 were retrospectively analyzed to identify risk factors of rebleeding. All patients were examined for risk factors and evaluated for increased hemorrhage by brain computed tomography at 3 days after surgery.
Results
This series included 54 men (32.5%) and 112 women (67.5%) of mean age 58.3┬▒14.3 years. After procedures, 26 patients (15.7%) experienced rebleeding, and 1 of these (0.6%) experienced an intraoperative aneurysmal rupture. External ventricular drainage (EVD) (odds ratio [OR] 5.389, [95% confidence interval (CI) 1.171-24.801]) and modified Fisher grade (OR 2.037, [95% CI 1.077-3.853]) were found to be independent risk factors of rebleeding, and perioperative rebleeding was strongly associated with patient outcomes (p’╝£0.001).
Aneurysmal Subarachnoid Hemorrhage (aSAH) is a fatal disease with high mortality and morbidity rates. According to several studies, the mortality rate of aSAH ranges from 8% to 67% [18], and in particular, the mortality rate in patients that experience rebleeding is as high as 80% [14,15]. In addition to rebleeding caused by aneurysmal re-rupture, delayed bleeding that occurs despite complete treatment of ruptured aneurysm often increases mortality and the frequencies of unfavorable outcomes such as disability and morbidity. Therefore, it is important to be aware of the risk factors of rebleeding and to evaluate and predict the risks of rebleeding at admission. Larger aneurysm size, increased systolic arterial blood pressure on admission, and high Hunt-Hess grade on arrival have been reported to be associated with an increased risk of rebleeding, but the risk factors of rebleeding remain controversial [2,7,14,17,19]. Therefore, the purpose of this study was to evaluate risk factors of rebleeding after endovascular treatment for aSAH and to identify those useful for determining monitoring and management strategies after surgery.
180 patients that underwent endovascular embolization with ruptured cerebral aneurysm by single neuro-interventionist at a single institution from January 2014 to December 2016 were studied retrospectively. All included patients underwent endovascular treatment within 6 hours after aneurysmal rupture. 14 patients were excluded from the study for the following reasons; 3 patients had deterioration of consciousness from preoperative brain computed tomography (CT) scan until immediately before surgery, 1 patient of confirming contrast leakage with rebleeding on procedural induced aneurysmal rupture during surgery, 1 patient of incomplete aneurysm coiling after endovascular treatment, 5 patients who were unable to perform subsequent brain CT scan because of unstable vital signs immediately after surgery, and lastly, there were 4 cases in which follow-up brain CT scans were not taken after surgery because the guardians did not want active treatment. So total 166 patients were enrolled in this study. We investigated age, gender, Hunt and Hess grade at presentation, aneurysmal size and location, preoperative Fisher and modified Fisher grades, intraoperative heparin loading, immediate postoperative external ventricular drainage (EVD) or lumbar drainage, and endovascular treatment techniques of all patients include in the study. In this study, the definition of rebleeding was defined as increased amount of subarachnoid hemorrhage (SAH), intracerebral hemorrhage (ICH), and intraventricular hemorrhage (IVH) on the follow-up brain CT scan performed 3 days after surgery compared to the brain CT scan performed immediately after surgery. Then, we examined whether there was an increased amount of bleeding on brain CT images taken immediately after surgery and 3 days after surgery compared to brain CT images taken immediately before surgery and analyzed the relation. This retrospective study was approved by the Institutional Review Board of Wonju Severance Christian Hospital (CR320164).
In all patients, endovascular treatment was performed under general endotracheal anesthesia. Diagnostic digital subtraction angiography and embolization were performed using an angiography unit Allura Xper FD-20 (Philips medical, Eindhoven, NLD). Three-dimensional rotational angiography was performed in all 166 patients to confirm aneurysm size and shapes. 5000 IUs (international units) of heparin were loaded through a femoral sheath at the beginning of the procedures at surgeonŌĆÖs discretion. During all 166 endovascular procedures, catheter flushing was maintained using a heparin/saline mix (5000 IU in 1 L of normal saline). Two surgeons who had performed the procedures were both neuro-interventionists with at least five years of experience. For each patient, the procedure techniques of single coiling, double microcatheter coiling, stent-assisted coiling and parent artery occlusion were determined according to the size and shape of the aneurysm. In all 166 cases, complete obliteration was achieved (Raymond-Roy occlusion classification class I). During the procedure, angiography was performed immediately after microcatheter positioning and coil insertion to check whether complications such as contrast leakage or thromboembolic event occurred. Patients were admitted to an intensive care unit (ICU) immediately after procedures and arterial blood pressure and electrocardiography were continuously monitored for at least a week. After surgery, in patients who underwent stent-assisted coil embolization were given dual antiplatelet medications (aspirin, clopidogrel) and only aspirin monotherapy was used in the patient who underwent simple coil embolization. Brain CT scan was performed immediately after procedures and 3 days later to check for rebleeding. Rebleeding was defined as an increase in the amount of SAH or the occurrence of new ICH, excluding contrast on follow-up brain CT scans.
The two-sample t-test or the chi-square test were used initially to identify associations with postoperative rebleeding, and logistic regression analysis was used to identify factors that independently predicted rebleeding and results are expressed as odds ratios (ORs) and 95% confidence intervals (CIs). Quantitative variable results are expressed as means┬▒standard deviations, and qualitative variable results as properties of variables. The analysis was conducted using SPSS (version 24.0. IBM Corp., Armonk, NY, USA), and statistical significance was accepted for p values ’╝£0.05.
Of the 166 total patients, 54 (32.5%) males and 112 (67.5%) females were enrolled, and the average age was 58.3┬▒14.3 years. (range from 27 to 90 years). There were 121 (72.9%) patients with preoperative Fisher grade 4, and there were 54 (32.5%) patients with modified Fisher grade 2 and 65 (39.2%) patients with modified Fisher grade 4. Ruptured aneurysm size was average 5.9┬▒2.8 mm. After the procedure, 26 patients (15.7%) showed an increase in hemorrhage on the follow-up brain CT scans, and one of them had aneurysmal rupture with contrast leakage during surgery. Table 1 summarizes the characteristics of the patients.
In the univariate analysis related to rebleeding, the age (p=0.601) and sex (p=0.506) of patients were not related, and the preoperative Glasgow Coma Scale (GCS) was lower in the rebleeding group (p=0.018). The Hunt and Hess grade was also higher in the rebleeding group at the time of admission to the emergency room (p=0.009), and the preoperative Fisher grade (p=0.011) and the modified Fisher grade (p=0.001) were higher in the rebleeding group. Aneurysm size (p=0.781), intraoperative heparin loading (p=0.782), and each endovascular treatment technique did not show statistical significance with rebleeding. However, the frequency of EVD (57.7% vs. 19.3%, p’╝£0.001) and decompressive craniectomy after endovascular treatment (26.9% vs. 5.7%, p=0.003) was high in the rebleeding group. The frequency of unfavorable outcome was higher (73.1% vs. 30.0%, p’╝£0.001) (Table 2).
However, in the results of multivariate analysis, only modified Fisher grade was identified as an independent factor related to rebleeding as a preoperative factor (OR 1.924, 95% CI [1.103-3.355]), and as a factor after endovascular treatment, only EVD was confirmed as an independent factor related to rebleeding (OR 4.636, 95% CI [1.412-15.217]). On the other hand, Fisher grade, preoperative GCS, preoperative Hunt and Hess grade, and decompressive craniectomy were not related to rebleeding (Table 3) (Fig. 1).
ASAH is a fatal disease that causes high mortality and morbidity. According to several studies, the mortality rate has been reported between 8% and 67%, and the mortality rate in patients with rebleeding has been reported as high as 80% [14,15,18,21]. After the occurrence of aSAH, rebleeding varies not only from re-rupture in the ruptured aneurysm, but also from the increase in the amount of hemorrhage found after successful repair of the ruptured aneurysm. The incidence of rebleeding during the first 72 hours after SAH was reported was 8-23%, and about 50-90% of rebleeding occurred within the first 6 hours after primary bleeding [1,3,7,8,11-14,19,24]. In addition, even after the most ambitious treatment protocol for ruptured aneurysm closure after primary bleeding, rebleeding rates of up to 15% during the first 6 hours have been reported [14]. In most previous studies, rebleeding has been defined as the occurrence of newly developed intracranial hematoma after closure of aneurysm on brain CT scan after the first bleeding [4,23]. This includes remote hemorrhage as well as patients with re-rupture of aneurysms. In this study, rebleeding was also defined as a case in which hemorrhage amount increased on follow-up brain CT scan after completion of the treatment of aSAH ruptured aneurysm.
The purpose of aneurysm occlusion after aSAH is to prevent rebleeding caused by re-rupture of the aneurysm. The mechanisms that cause rebleeding are complex and influenced by many factors. Although several studies have been conducted on risk factors that increase the risk of rebleeding of aSAH, not all studies have reported consistent conclusions, and for this reason, the risk factors related to rebleeding are still controversial [14]. van Donkelaar et al. [25] suggested that high World Federation of Neurosurgical Societies (WFNS) grade at hospitalization, large size aneurysm of 20 mm or more (adjusted harzard ratio (aHR) 4.4, 95% CI [1.6-13.2]), modified Fisher grade 3 or higher (aHR 4.7, 95% CI [2.1-10.6]) and EVD (aHR 1.7, 95% CI [1.4-2.5]) were reported as risk factors for aSAH rebleeding. On the other hand, Wu et al26). reported that when the cut off value of the cerebral aneurysm diameter was 7 mm, the risk of rebleeding was significantly increased in the group of 7 mm or more (19.4% vs. 6.8%, p=0.0487), but Fisher grade and WFNS score did not significantly increase the risk of rebleeding (p=0.6122, 0.4580). In the case of Hunt and Hess grades, some studies showed that the higher the grade, the higher the risk of rebleeding, while there were cases with insignificant correlation [12,14,17].
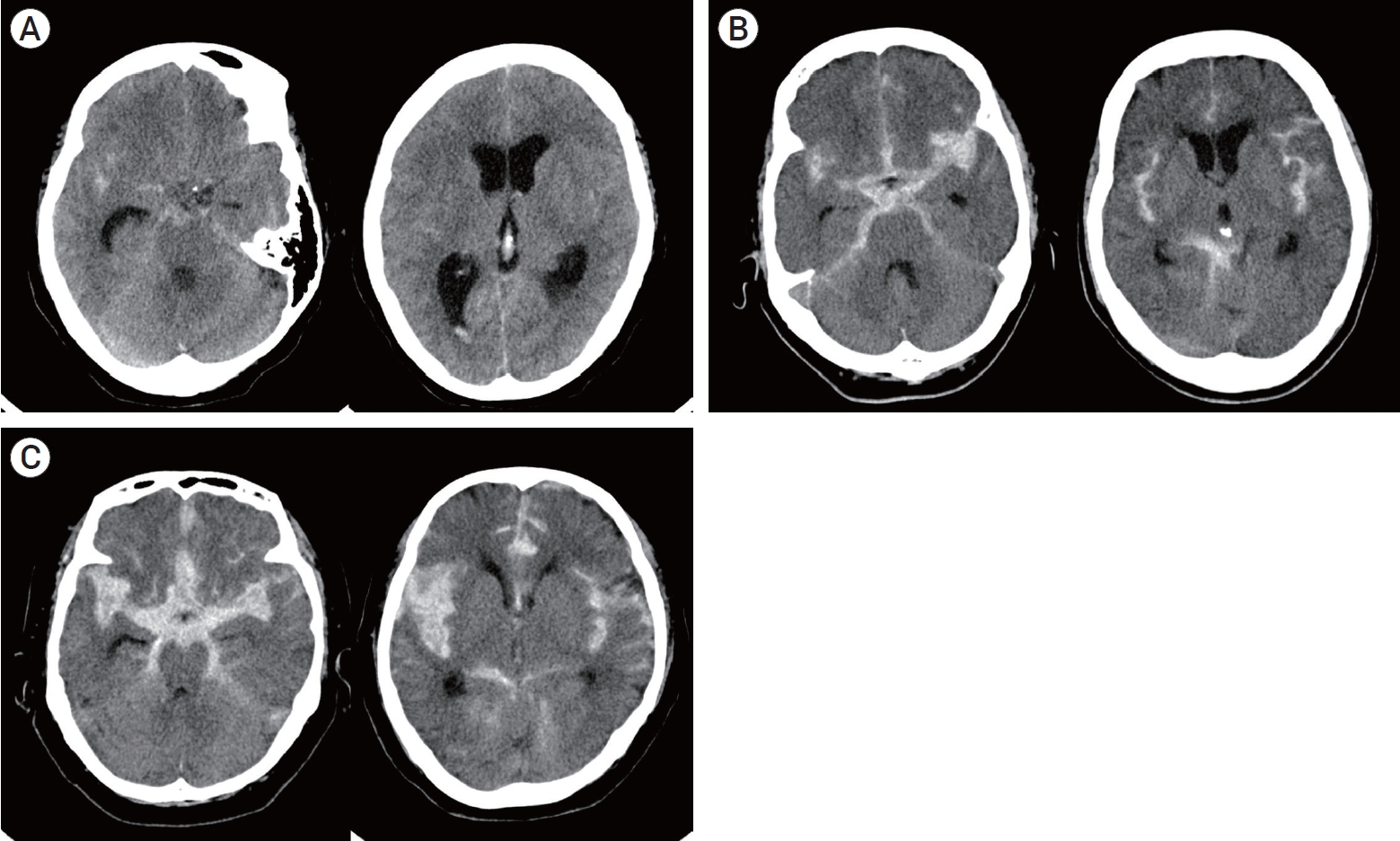
Fisher grade was first proposed by Fisher et al. in 1980, and radiologically grading the amount of hemorrhage present in cistern after aneurysmal SAH occurrence [5,6]. In general, Fisher grade has been widely used to evaluate the risk of delayed cerebral ischemia (DCI) because the amount of SAH present in cistern after aSAH shows the greatest correlation with the occurrence of DCI caused by vasospasm [5]. Fisher grade evaluates the risk of DCI through the amount of cisternal blood and the presence of IVH and ICH. If thick cisternal blood is shown, it is classified as Grade 3, and if ICH or IVH is present, it is classified as Grade 4, but the risk of DCI occurrence of ICH and IVH cannot be distinguished. Therefore, in 2001, Claassen et al. [5] reported that thick clot completely filling any cistern or fissure is the strongest risk factor for DCI and that the presence of IVH in both lateral ventricles has a strong correlation through a study on the possibility of DCI after aSAH. Also, based on the fact that the presence or absence of thick cisternal SAH and IVH acts as an additive risk factor for DCI, a modified Fisher scale was newly proposed according to the presence or absence of thick SAH and IVH (Table 4). In other words, it can be said that the modified Fisher grade reflects the amount of hemorrhage more accurately than the Fisher grade (Fig. 2).
Ando et al. [1] proposed the hypothesis that the risk of rebleeding can be increased by interfering with the solidifying of blood clots when the aneurysm dome is embedded in the thick hematoma mass. and based on this, Ando et al. argued that the higher the modified Fisher scale, which is a measure that can intuitively reflect the amount of intracranial hematoma, is associated with the occurrence of rebleeding. In addition, van Donkelaar et al. [25] reported that the amount of blood acted as a surrogate marker of the defect size and stability of the ruptured aneurysm wall, showing a high correlation with the occurrence of rebleeding within 24 hours when the modified Fisher grade was 3 to 4 (aHR 4.7, 95% CI [2.1-0.6]). In addition, Hilditch et al. [10] reported a case of rupture of small pial branches of sylvian middle cerebral artery by expansion of sylvian fissure hematoma after acute post-aSAH, causing remote multifocal bleeding, resulting in the formation of hematoma in the sylvian subpial space. As a result, it was argued that there is a relationship between hematoma amount and remote hemorrhage, as the greater the amount of SAH caused by ruptured aneurysm, the greater the expanding effect of sylvian fissure and the likelihood of the occurrence of remote subpial bleeding will increase. Although these studies have different hypotheses, it can be said that they have in common argued the relationship between large amount hemorrhage and aSAH rebleeding.
Many studies have reported that SAH rebleeding is related to the extra ventricular drainage. In general, it is known that the hypothesis that rapid regulation of intracranial pressure (ICP) through EVD reduces the tamponade effect acting on recently ruptured aneurysm leading to rebleeding is the most reliable. This causes a decrease in ICP while cerebrospinal fluid (CSF) drainage through the EVD, which is known to increase the transmural pressure, which may exacerbate the risk of rebleeding. However, it is still not supported as solid evidence that CSF drainage increases the risk of rebleeding [9,14,16,20,22]. van Donkelaar et al. [25] reported initiation of EVD as a risk factor for rebleeding (aHR 1.9, 95% CI [1.4-2.5]). Similarly, Naidech et al. [17] reported whether EVD was implemented as a risk factor for rebleeding (OR 5.10, 95% CI [1.62-15.99]). but This study was limited to patients who were relatively good neurologic grade Hunt and Hess grade I to III at the time of admission, as a result, the authors said that it was a result with limitations in that it was not possible to exclude the case where EVD was performed because the patient worsened after the occurrence of rebleeding. In our study, it was concluded that the EVD implementation was related to rebleeding. However, in this institution, because EVD was performed when the large amount of hemorrhage or massive IVH was accompanied, the increase in risk of rebleeding becaused of the condition in which the amount of hemorrhage was high before EVD could not be excluded. Therefore, there is a problem in concluding that the rebleeding risk has increased by the implementation of EVD itself.
This study is inherently limited by its non-randomized, retrospective, single center design and the relatively small number of cases included, which limit the generalizabilities of our findings.
On the other hand, since we performed ultra-early endovascular intervention within about 2 to 3 hours for all aSAH patients, rebleeding caused by aneurysm re-rupture that occurred between the initial brain CT angiography and the end of the intervention was excluded as exclusion criteria. Thus, it is a strength of this study that selective statistical analysis of patients with rebleeding, that is, remote hemorrhage, set in this study was possible.
If rebleeding occurs during aSAH treatment, it shows a high morbidity and mortality. For this reason, more careful monitoring and treatment are required in the case of the patient group with a risk factor associated with the occurrence of rebleeding after aSAH. According to this study, in the case of high modified Fisher grade on brain CT scan and accompanied by thick IVH requiring EVD, the risk of remote rebleeding after surgery is high. Therefore, more careful monitoring in the ICU is required during aSAH treatment.
Fig.┬Ā1.
Forest plot on the relationship between the rebleeding risk after endovascular treatment and pre/postoperative risk factors.
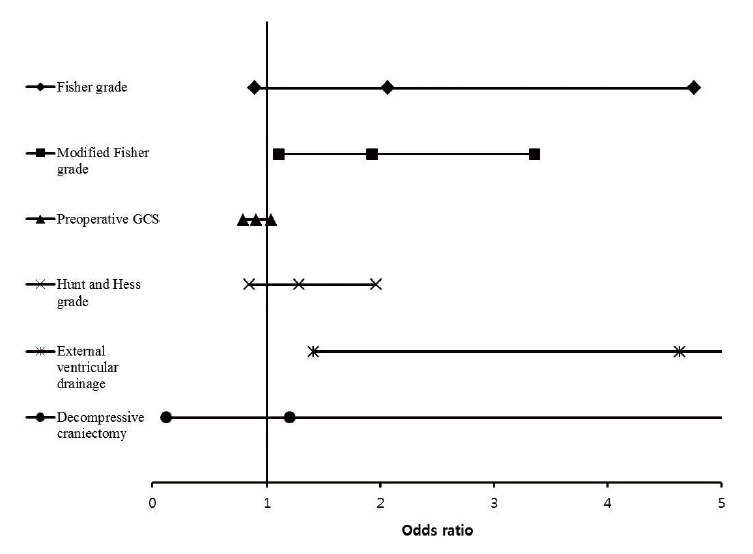
Fig.┬Ā2.
(A) This patient had a small amount of SAH, but with IVH, and was classified as grade 4 for Fisher grade and grade 2 for modified Fisher grade. (B) This patient showed thick SAH without IVH and was classified as grade 3 in both Fisher and modified Fisher grades. (C) This patient was classified as grade 4 for both Fisher grade and modified Fisher grade as thick SAH with IVH. Compared with (A) and (C), although the absolute amount of hemorrhage shows a remarkable difference, the Fisher grade was all grade 4, and the difference in absolute hemorrhage amount was not distinguishable, but the modified Fisher grade was classified as grade 2 and 4, reflecting the hemorrhage amount. Compared with A and B, the absolute amount of hemorrhage is higher in B, but in Fisher grade, (A) was higher as grade 4, whereas in modified Fisher grade, grade increased as the amount of hemorrhage increases in the order of (A), (B) and (C). SAH, subarachnoid hemorrhage; IVH, intraventricular hemorrhage.
Table┬Ā1.
Characteristics of 166 patients underwent coil embolization with aneurysmal subarachnoid hemorrhage
Table┬Ā2.
Univariate analysis of baseline variables associated with postoperative rebleeding
Table┬Ā3.
ORs of rebleeding after endovascular treatment for pre/post operative risk factors
| Crude OR (95% CI) | Adjusted OR* (95% CI) | Adjusted ORŌĆĀ (95% CI) | |
|---|---|---|---|
| Fisher grade | 1.747 (0.938-3.253) | 1.723 (0.922-3.222) | 2.064 (0.894-4.761) |
| Modified Fisher grade | 1.839 (1.236-2.738) | 1.926 (1.263-2.939) | 1.924 (1.103-3.355) |
| Preoperative GCS | 0.875 (0.792-0.966) | 0.874 (0.790-0.967) | 0.905 (0.788-1.039) |
| Hunt and Hess grade | 1.487 (1.092-2.025) | 1.489 (1.086-2.042) | 1.285 (0.843-1.961) |
| External ventricular drainage | 5.707 (2.358-13.815) | 5.978 (2.439-14.651) | 4.636 (1.412-15.217) |
| Decompressive craniectomy | 6.079 (1.978-18.680) | 6.083 (1.957-18.915) | 1.202 (0.114-12.677) |
Table┬Ā4.
Fisher grade and modified Fisher grade
| Fisher grade | Modified Fisher grade | |
|---|---|---|
| 0 | No SAH or IVH | |
| 1 | No blood detected | Minimal/thin SAH, no IVH in either lateral ventricle |
| 2 | Diffuse deposition of thin layer with all vertical layers of blood less than 1 mm thick | Minimal/thin SAH, with IVH in both lateral ventricles |
| 3 | Localized clots and/or vertical layers of blood 1 mm or more in thickness | Thick SAH,* no IVH in either lateral ventricle |
| 4 | Intracerebral or intraventricular with diffuse or no subarachnoid blood | Thick SAH,* with IVH in both lateral ventricles |
REFERENCES
1. Ando T, Sakai N, Yamada H, Iwai T, Nishimura Y, Hirata T, et al. Analysis of reruptured cerebral aneurysms and the prophylactic effects of barbiturate therapy on the early stage. Neurol Res. 1989 Dec;11(4):245-8.


2. Beck J, Raabe A, Szelenyi A, Berkefeld J, Gerlach R, Setzer M, et al. Sentinel headache and the risk of rebleeding after aneurysmal subarachnoid hemorrhage. Stroke. 2006 Nov;37(11):2733-7.


3. Cha KC, Kim JH, Kang HI, Moon BG, Lee SJ, Kim JS. Aneurysmal rebleeding : factors associated with clinical outcome in the rebleeding patients. J Korean Neurosurg Soc. 2010 Feb;47(2):119-23.



4. Choi J, Koo Y, Whang K, Cho S, Kim J. Safety of heparin loading during endovascular embolization in patients with aneurysmal subarachnoid hemorrhage. Clin Neurol Neurosurg. 2021 Feb;201:106453.


5. Claassen J, Bernardini GL, Kreiter K, Bates J, Du YE, Copeland D, et al. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: the Fisher scale revisited. Stroke. 2001 Sep;32(9):2012-20.


6. Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980 Jan;6(1):1-9.


7. Fujii Y, Takeuchi S, Sasaki O, Minakawa T, Koike T, Tanaka R. Ultra-early rebleeding in spontaneous subarachnoid hemorrhage. J Neurosurg. 1996 Jan;84(1):35-42.


8. Gruber A, Dietrich W, Czech T, Richling B. Recurrent aneurysmal subarachnoid haemorrhage: bleeding pattern and incidence of posthaemorrhagic ischaemic infarction. Br J Neurosurg. 1997 Apr;11(2):121-6.


9. Hellingman CA, van den Bergh WM, Beijer IS, van Dijk GW, Algra A, van Gijn J, et al. Risk of rebleeding after treatment of acute hydrocephalus in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2007 Jan;38(1):96-9.


10. Hilditch CA, Sonwalkar H, Wuppalapati S. Remote multifocal bleeding points producing a Sylvian subpial hematoma during endovascular coiling of an acutely ruptured cerebral aneurysm. J Neurointerv Surg. 2017 Jul;9(7):e25.


11. Hillman J, von Essen C, Leszniewski W, Johansson I. Significance of ŌĆ£ultra-earlyŌĆØ rebleeding in subarachnoid hemorrhage. J Neurosurg. 1988 Jun;68(6):901-7.


12. Inagawa T, Kamiya K, Ogasawara H, Yano T. Rebleeding of ruptured intracranial aneurysms in the acute stage. Surg Neurol. 1987 Aug;28(2):93-9.


13. Kitsuta Y, Suzuki N, Sugiyama M, Yamamoto I. Changes in level of consciousness and association with hyperglycemia as tool for predicting and preventing re-bleeding after spontaneous subarachnoid hemorrhage. Prehosp Disaster Med. 2006 May-Jun;21(3):190-5.


14. Larsen CC, Astrup J. Rebleeding after aneurysmal subarachnoid hemorrhage: a literature review. World Neurosurg. 2013 Feb;79(2):307-12.


15. Lovelock CE, Rinkel GJ, Rothwell PM. Time trends in outcome of subarachnoid hemorrhage: Population-based study and systematic review. Neurology. 2010 May;74(19):1494-501.



16. McIver JI, Friedman JA, Wijdicks EF, Piepgras DG, Pichelmann MA, Toussaint LG, et al. Preoperative ventriculostomy and rebleeding after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2002 Nov;97(5):1042-4.


17. Naidech AM, Janjua N, Kreiter KT, Ostapkovich ND, Fitzsimmons BF, Parra A, et al. Predictors and impact of aneurysm rebleeding after subarachnoid hemorrhage. Arch Neurol. 2005 Mar;62(3):410-6.


18. Nieuwkamp DJ, Setz LE, Algra A, Linn FH, de Rooij NK, Rinkel GJ. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol. 2009 Jul;8(7):635-42.


19. Ohkuma H, Tsurutani H, Suzuki S. Incidence and significance of early aneurysmal rebleeding before neurosurgical or neurological management. Stroke. 2001 May;32(5):1176-80.


20. Pare L, Delfino R, Leblanc R. The relationship of ventricular drainage to aneurysmal rebleeding. J Neurosurg. 1992 Mar;76(3):422-7.


21. Rivero Rodr├Łguez D, Scherle Matamoros C, C├║e LF, Miranda Hern├Īndez JL, Pernas S├Īnchez Y, P├®rez Nellar J. PredictorŌĆÖs of mortality in patients with aneurysmal subarachnoid haemorrhage and reebleding. Neurol Res Int. 2015 2015:545407.



22. Ruijs AC, Dirven CM, Algra A, Beijer I, Vandertop WP, Rinkel G. The risk of rebleeding after external lumbar drainage in patients with untreated ruptured cerebral aneurysms. Acta Neurochir (Wien). 2005 Nov;147(11):1157-61; discussion 1161.


23. Tang C, Zhang TS, Zhou LF. Risk factors for rebleeding of aneurysmal subarachnoid hemorrhage: a meta-analysis. PLoS One. 2014 9(6):e99536.



24. Tanno Y, Homma M, Oinuma M, Kodama N, Ymamoto T. Rebleeding from ruptured intracranial aneurysms in North Eastern Province of Japan. A cooperative study. J Neurol Sci. 2007 Jul;258(1-2):11-6.


-
METRICS

-
- 2 Crossref
- 0 Scopus
- 3,364 View
- 93 Download
- ORCID iDs
-
Jongwook Choi

https://orcid.org/0000-0003-2593-3870 - Related articles
-
Preoperative Grading Systems of Spontaneous Subarachnoid Hemorrhage.2000 March;2(1)
General Complications of Aneurysmal Subarachnoid Hemorrhage.2001 March;3(1)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



