 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 25(2); 2023 > Article |
|
Abstract
Objective
Dual antiplatelet therapy (DAPT) is usually temporarily used after stent-assisted coil embolization (SACE), and is commonly converted to mono antiplatelet therapy (MAPT) for indefinitely. In this study, we aimed to find the possibility of discontinuing MAPT, and to determine the proper period of DAPT use.
Methods
We used the Standard Sample Cohort DB dataset from the National Health Insurance Sharing Service. Among approximately 1 million people in the dataset, SACE was performed in 214 patients whose data this study analyzed. The relationship between discontinuation of antiplatelet therapy and intracranial hemorrhage or cerebral infarction was analyzed using multiple logistic regression, considering all confounding variables. The survival rate according to the continuation of antiplatelet therapy was obtained using Kaplan-Meier analysis, and the difference in survival rate according to the continuation of antiplatelet therapy was verified using the log-rank test. The hazard ratio according to continuation of antiplatelet therapy was obtained using the Cox proportional hazards model. The analysis was conducted by applying the same statistical method to the duration of DAPT use.
Results
Among 214 patients who underwent SACE, 50, 159 and five patients continued, discontinued and did not use antiplatelet therapy (except at the time of procedure), respectively. In multiple logistic regression analysis, discontinuation of antiplatelet agents (including aspirin) and the period of DAPT use did not affect the occurrence of intracranial hemorrhage or cerebral infarction, considering various confounding factors. In the survival analysis according to the continuation of antiplatelet agents, patients who continued to use antiplatelet agents had a higher survival rate than those in other groups (p=0.00). The survival rate was higher in the rest of the group than in the group that received DAPT for three months (p=0.00).
Conclusions
Continuation of antiplatelet agents or the period of DAPT use did not affect the occurrence of intracranial hemorrhage or cerebral infarction. Considering the survival rate, it would be better to maintain at least three months of antiplatelet therapy and it might be recommended to continue DAPT use for 12 months.
Stent-assisted coil embolization (SACE) is an effective endovascular treatment for wide-neck aneurysms. Stents facilitate aneurysm coiling and provide long-lasting aneurysm obliteration more than coil embolization alone [1,4]. However, using a stent can cause thromboembolism during and after coil embolization, and more frequently can lead to cerebral ischemic events [3,10,19]. Therefore, antiplatelet agents were initiated before embolization and continued after the procedure. Usually, dual antiplatelet therapy (DAPT) is temporarily used after SACE, and is then commonly converted to mono antiplatelet therapy (MAPT) for life. The period of continuing DAPT was slightly different for each physician and institution. A shorter period may increase the likelihood of thromboembolism and, on the contrary, a longer period may increase the possibility of intracranial hemorrhage. In recent years, it has been suggested that the DAPT continuation period should be extended to nine months in order to further lower thromboembolism risk [12]. Although it is common to continue to use DAPT for six weeks to six months, little research has been conducted on the proper length of DAPT use [2,13,17,18,20].
In addition, few studies have been conducted on MAPT discontinuation. It is a common recommendation to maintain MAPT for the rest of one’s life after SACE. However, many researchers have questioned whether the maintenance of MAPT for a lifetime in patients undergoing SACE without vasculopathy such as atherosclerosis is a good choice, and there is an opinion that MAPT can be stopped after a certain period of time [7,11].
Since this subject is directly related to the treatment outcome and prognosis of the patient, there is no randomized controlled trial (RCT) on this subject. There are also few case-control studies, and case series accounts for most of it [7,11,12]. Therefore, this study aimed to determine the possibility of discontinuing MAPT by comparing the subsequent thromboembolism, intracranial hemorrhage, and mortality between the group that discontinued MAPT (for any reason) and the group that continued MAPT in post-SACE patients. In addition, we classified the patients who underwent SACE according to the period of DAPT use and compared thromboembolism, intracranial hemorrhage, and mortality in each group to determine the proper period of DAPT use. These findings may help guide establishing antiplatelet therapy in patients who have undergone SACE.
This study used the Standard Sample Cohort DB dataset from the National Health Insurance Sharing Service. Standard sample cohort DB data were extracted from the patient unit stratification system based on sex, age, income level, and regional classification. It also included details of the care and prescription(s) for all Koreans who used hospital services throughout Korea over a 14-year period (2002-2015). The extraction rate is approximately 2.1%, which is approximately 1 million out of 46 million Koreans who were eligible for National Health Insurance in 2006. Among these, patients who did not have any data necessary for analysis of the Standard Sample Cohort DB were excluded. Endovascular coil embolization was performed in 812 patients, and data on these 812 patients (250 men and 562 women) were analyzed. Among 812 patients, SACE was performed in 214 patients, of whom the data was analyzed. We did not analyze the data according to the ruptured and unruptured aneurysm.
The dependent variable was intracranial hemorrhage or cerebral infarction, and only patients who were hospitalized with these diagnoses were included. Intracranial hemorrhage or cerebral infarction was classified as either present or absent, and patients who had hemorrhage or infarction after SACE procedures were included. The Korean Classification of Diseases (KCD) code used to diagnose intracranial hemorrhage and cerebral infarction is described in Table 1 and is based on the disease name file published on July 27, 2017.
The independent variables were continuation of antiplatelet agent use and the duration of DAPT use. The confounding variables included sex, age, diabetes, hypertension, cardiovascular disease, use of low-dose aspirin (less than 100 mg), other antiplatelet agents, anticoagulants, NSAIDs, aspirin as an analgesic (more than 500 mg), systemic corticosteroids, selective serotonin reuptake inhibitors (SSRIs), proton pump inhibitors (PPIs), and HMG-CoA reductase inhibitors (statins). Drugs were divided into used or unused, and the drug code was based on the list of drugs published on March 1, 2019, and are described in Table 2. The diseases were classified as present or absent, and the diagnostic code for each disease was based on the previous KCD code table on July 27, 2017 (Table 1).
The relationship between discontinuation of antiplatelet therapy and intracranial hemorrhage or cerebral infarction was analyzed using multiple logistic regression, considering all confounding variables. The odds ratio (OR) and 95% confidence interval (CI) were calculated, and the statistical significance level was set at 0.05. The survival rate according to the continuation of antiplatelet therapy was obtained using Kaplan-Meier analysis, and the difference in survival rate according to the continuation of antiplatelet therapy was verified using the log-rank test, a nonparametric test method. In addition, the hazard ratio according to continuation of antiplatelet therapy was obtained using the Cox proportional hazards model. The analysis was conducted by applying the same statistical method as described above to the period of DAPT use. R software (version 3.6.1; R Project for Statistical Computing, Vienna, Austria) was used for analysis’ the “dplyr” package was used for data cleansing; “moonBook” packages were used for multiple logistic regression analysis; “survminer” and “survival” packages were used for the survival analysis.
The average age of the patients who underwent endovascular coil embolization was 57.75±12.13 years in total i.e., 53.8±12.42 years for men, and 59.51±11.59 years for women. Among 812 patients, endovascular coil embolization assisted by stent (SACE) was performed in 214 patients, endovascular coil embolization assisted by other devices in 165 patients, and simple endovascular coil embolization in 433 patients. Among 214 patients who underwent SACE, 50, 159, and five patients continued, discontinued, and did not use antiplatelet therapy except at the time of procedures, respectively (Table 3). Among 165 patients who underwent endovascular coil embolization assisted by other devices, 16, 131, and 18 patients continued, discontinued, and did not use antiplatelet therapy except at the time of procedures, respectively (Table 3). Among 433 patients who underwent simple endovascular coil embolization, 31, 292, and 110 patients continued, discontinued, and did not use antiplatelet therapy except at the time of the procedure, respectively (Table 3).
The ORs and 95% CIs for intracranial hemorrhage from this multiple logistic regression analysis are summarized in Table 4. As shown in Table 4, the p-value in the rightmost column was greater than 0.05 (not statistically significant) for all variables. Therefore, discontinuation of antiplatelet agents (including aspirin) did not affect the occurrence of intracranial hemorrhage considering various confounding factors.
The ORs and 95% CIs for cerebral infarction from this multiple logistic regression analysis are summarized in Table 5. As shown in Table 5, the p-value in the rightmost column was more than 0.05 (not statistically significant) for all variables except for DAPT use for over 13 months, and antiplatelet agents other than aspirin. If DAPT was used for over 13 months, the possibility of cerebral infarction was 273 times higher, and if antiplatelet agents other than aspirin were used, the possibility of cerebral infarction was reduced by 0.03 times. Eventually, discontinuation of antiplatelet agents (including aspirin) did not affect the occurrence of cerebral infarction owing to various confounding factors.
In patients who underwent SACE, survival analysis according to continuation of antiplatelet agents was performed using Kaplan-Meier analysis (Fig. 1). Patients who continued to use antiplatelet agents had a higher survival rate than those who discontinued antiplatelet agents, and the survival rate of these two groups was higher than those who did not use antiplatelet agents except at the time of procedure.
These differences in survival rates among the three groups according to the continuation of antiplatelet agents were tested using the log-rank test (X2=58.7, p=0.00) indicating statistically significant differences in survival rates. The differences in survival rates between the groups who continued and discontinued antiplatelet agents were tested using the log-rank test (X2=4.1, p=0.0422), indicating significant statistical differences in survival rates between the two groups.
The hazard ratio was calculated using the Cox proportional risk model according to the continuation of antiplatelet agents. The mortality risk of the group that discontinued antiplatelet agents was 7.281e+07 times compared to the group that continued to use antiplatelet agents, and the mortality risk of the group that did not use antiplatelet agents except for the time of procedures was 1.331e+09 times. The results were similar even when comparing the two groups that continued or discontinued antiplatelet agents, and the mortality risk of the group that discontinued antiplatelet agents was 2.759e+08 times compared to the group that continued to use antiplatelet agents.
In patients who underwent SACE, survival analysis according to the period of DAPT use was performed using Kaplan-Meier analysis (Fig. 2). The survival rate seemed to be higher in the rest of the group than in the group that received DAPT for three months. These differences in survival rates among the five groups were tested using the log-rank test, and X2=28.6 and p=0.00, indicating significant statistical differences in survival rates. The hazard ratio was calculated using the Cox proportional risk model according to the period of DAPT use, and the group using DAPT for less than three months was set as the basis and compared. Compared to the group that used DAPT for less than three months, the mortality risk was 0.1707, 0.1844, 4.323e-09, and 0.04528 times in the group that used DAPT for less than six, nine, and 12 and more than 13 months, respectively.
In this study, we extracted 812 patients who underwent endovascular coil embolization for cerebral aneurysms out of 1 million people from Standard Sample Cohort DB datasets. Among the 812 patients, 214 who underwent SACE for cerebral aneurysms were extracted and analyzed. Before the analysis, we thought that many patients would be identified because of the 1 million people data extraction pool, but a relatively low frequency of 214 was detected. It is judged that the endovascular SACE was relatively less frequently performed between 2002 and 2015, which is the subject of this study. Therefore, if it can be applied to the recent period as a protocol of this study, the study population may be increased, and subsequently further study may be needed.
The 214 patients who underwent SACE were divided into three groups: (1) continued use of antiplatelet agents (n=50), (2) discontinued antiplatelet use at a certain time (reasons unknown) (n=159), and (3) no use of antiplatelet agents (n=5), except at the time of procedures. A lifetime use of antiplatelet agents is usual. In this study, the number of patients with discontinued antiplatelet therapy was around three times higher than those who continued to use antiplatelet agents (159/50=3.18). In other words, although the exact reason is unknown, it was confirmed that antiplatelet agent use was discontinued in more patients than expected. Of course, this ratio is smaller than in the group (135/16=8.44 times) that underwent endovascular coil embolization assisted by other devices such as balloon-assisted coil embolization and the group (292/31=9.42 times) that underwent only endovascular coil embolization, which is consistent with common sense (Table 3).
Among these three groups, multivariate analysis including various confounding variables was conducted to determine the effect of continuation of antiplatelet agents on intracranial hemorrhage or cerebral infarction. As previous studies have reported an increased risk of bleeding due to antiplatelet use, the risk of intracranial hemorrhage could be higher in patients who continue to use antiplatelet agents than in other groups [6,8,9,16]. However, in this study, the continuation of antiplatelet agents did not affect intracranial hemorrhage (p>0.05) (Table 4). In addition, DAPT use may also increase the risk of intracranial hemorrhage; however, in this study, the difference in the duration of DAPT use was not related to the risk of intracranial hemorrhage (p>0.05) (Table 4). Although most studies have also shown that antiplatelet agents increase the risk of intracranial hemorrhage, in some studies, the use of low-dose aspirin was not related to intracranial hemorrhage, and this study also produced results in this context [5,14,21]. Considering these results, the use of antiplatelet agents and the period of DAPT use are not related to intracranial hemorrhage; therefore, it might not be necessary to discontinue antiplatelet agents because of concerns of bleeding, including intracranial hemorrhage.
Since antiplatelet agents are usually used as secondary preventive agents for cerebral infarction [15], the risk of cerebral infarction was expected to be lower in patients who continued to use antiplatelet agents than in patients who discontinued antiplatelet agents in this study. In contrast, the risk of cerebral infarction was expected to be higher in patients who discontinued than in those who continued antiplatelet agent use.
Nonetheless, in this study, discontinuation of antiplatelet agents was not associated with the risk of cerebral infarction (p>0.05) (Table 5). In other words, when stents are used in cerebral aneurysms, it is not necessary to prolong antiplatelet agents for cerebral infarction prevention, which may seem to be due to the fact that the basic pathology of cerebral aneurysms is different from atherosclerosis. Several studies have reported similar results. In 2022, Goto et al. reported that discontinuation of antiplatelet agents was performed in 147 (71.7%) of 205 patients who underwent SACE and were followed for more than two years with no cerebral ischemic complications. Therefore, they suggested that discontinuation of antiplatelet agents should be cautiously considered [7]. In 2022, Hong et al. also reported similar results, in which the discontinuation of antiplatelet agents was performed in 74 (61.6%) of 120 patients who underwent SACE and were followed for more than six months with no cerebral ischemic complications. Therefore, they also suggested that it may be safe to discontinue antiplatelet agents after SACE in patients at low risk for ischemia, and the optimal time to discontinue might be around 18-36 months after SACE [11].
The risk of cerebral infarction according to the period of DAPT use was 273 times higher (p=0.035) in patients who used DAPT for over 13 months than in other groups, which is contrary to the established fact. This group continued to use DAPT for over 13 months, which is longer than the typical period because cerebral atherosclerosis was thought to be very severe. In other words, it is estimated that DAPT was continued for over 13 months, not simply because the stent was used, but also because cerebral atherosclerosis was severe. Therefore, it would be natural to show a higher risk of cerebral infarction in this group. In addition, the use of antiplatelet agents other than aspirin reduced the risk of cerebral infarction (0.03 times, p=0.017), which is consistent with the established fact that antiplatelet agents reduce the risk of cerebral infarction.
The survival rate was higher in patients who continued than those who discontinued the use of antiplatelet agents, or those who did not use antiplatelet agents except for at time of procedures, and the survival rate of patients who discontinued antiplatelet agents was also higher than in those who did not use antiplatelet agents except at the time of procedures (p<0.0001). These risks would have been high because the death rate of the group that continued to use antiplatelet agents was zero. However, in terms of the risk of death, it may be better to continue antiplatelet agent use. As mentioned above, the continuation of antiplatelet agents does not have much to do with intracranial hemorrhage or cerebral infarction in the group with SACE for cerebral aneurysm, but the continuation of antiplatelet agents is thought to affect the survival rate of patients in that group due to other unexplained factors.
In the survival analysis according to the period of DAPT use, the survival rate of patients was higher in all groups with more than three months than in the group with less than three months of antiplatelet therapy (p=0.00). Compared to the group that continued to use DAPT for less than three months, the mortality risk of patients who continued it up to six, nine, and 12 months and more than 13 months months was 0.1707, 0.1844, 4.323e-09, and 0.04528 times respectively. That is, the mortality risk was lowest and highest in the group that continued antiplatelet therapy up to 12 and nine months, respectively. Thus, it was suggested that the period of DAPT was not significantly related to the occurrence of intracranial hemorrhage or cerebral infarction. Therefore, although we could not explain the exact reason, it might be better to continue DAPT use for at least three months for patient survival, while continuation for up to 12 months might be more advantageous.
This study has several limitations. As mentioned above, this study was based on insurance claims, with limited reliability of the accuracy of the specific diagnosis. Moreover, our data included only patients with at least one hospitalization experience for intracranial hemorrhage or cerebral infarction. In the case of insurance claims, the diagnosis code can be entered even if there is only suspicion, and there is a possibility that the diagnosis code remains even if the suspicion is not confirmed. In patients with hospitalization experience, the diagnostic codes may be more accurate; however, the addition of more diagnostic codes and medicines can be expected to cause more confusion in the results. To overcome these limitations, we included patients who were admitted with a diagnosis, including the 5th priority in the diagnosis of diseases. Nevertheless, there are still limitations but a more accurate result may be obtained if further studies are conducted to improve the operational definition of the disease. For example, the definition of disease is defined by using a drug for the disease and not only the diagnosis code; If the diagnosis code priority of disease is lowered over 5th priority for example 7th or 10th, or is not only with regards to hospitalized patients for intracranial hemorrhage, but also to outpatients, the target group is increased. In addition, for the prescription period of antiplatelet agents, we can know the date of prescription, but we do not know the number of days the agents were prescribed. Therefore, this study set a maximum prescription period of three months, but in fact it may be six months, so there may be an error in the study. These limitations can usually be overcome in large-scale data research; however, since this study was conducted on a smaller number of patients than initially expected, the credibility of this study is inevitably reduced. This is expected to be overcome if the study is conducted using more data in the future.
The continuation of antiplatelet agents did not affect the occurrence of intracranial hemorrhage or cerebral infarction; however, the survival rate of the group that continued antiplatelet agents was higher than that of other groups. The period of DAPT use did not affect the occurrence of intracranial hemorrhage or cerebral infarction, but the mortality risk in the group that continued for up to three months was the highest, so it would be better to maintain it for at least three months. Statistically, it might be recommended to continue DAPT use for 12 months because the survival rate was the highest in the group that continued DAPT use for 12 months.
NOTES
ACKNOWLEDGEMENTS
This research was supported by Korean NeuroEndovascular Society research fund (Kones-2020-04).
Fig. 1.
Survival analysis according to the continuation of antiplatelet agents.
SubGroup 0 - continued antiplatelet use, SubGroup 1 - discontinued antiplatelet use, SubGroup 2 - no platelet use The unit of time is a month.
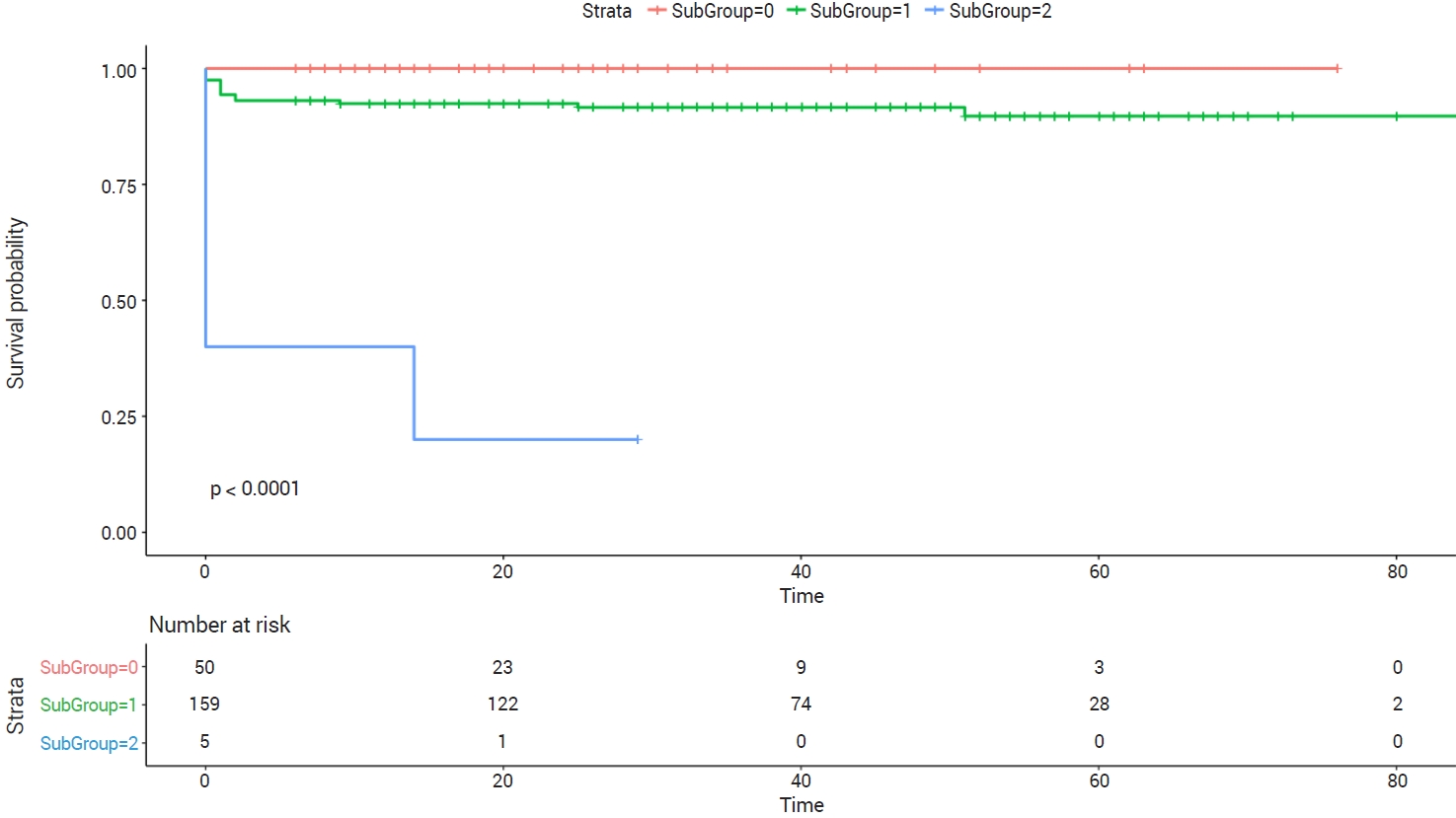
Fig. 2.
Survival analysis according to the period of DAPT use.
DAPTG 3, 6, 9, 12, 13 - dual antiplatelet therapy (DAPT) use for less than three, six, nine, 12, and over 13 months The unit of time is a month.

Table 1.
Diagnostic code for each disease
Table 2.
Drug code for each drug
Table 3.
The types of endovascular coil embolization and antiplatelet use
Table 4.
Adjusted odds ratios and 95% confidence intervals from multiple logistic regression in intracranial hemorrhage*
| Variables | Adjusted OR | 95% CI | p-value |
|---|---|---|---|
| (Intercept) | 0.00 | 0 - Inf | 0.9998 |
| Gender† | 2.83 | NA - Inf | 1.0000 |
| AgeOp†† | 12.48 | 0 - 2.502315e+66 | 0.9985 |
| SubGroup 1††† | 0 | NA - Inf | 0.9999 |
| SubGroup 2††† | 0 | 0 - Inf | 1.0000 |
| DAPTG 6†††† | 0 | 0 - Inf | 0.9998 |
| DAPTG 9†††† | 0 | NA - Inf | 0.9999 |
| DAPTG 12†††† | 222.97 | 0 - Inf | 1.0000 |
| DAPTG 13†††† | 0 | 0 - Inf | 0.9998 |
| Diabetes | 2.15 | 0 - Inf | 1.0000 |
| Hypertension | 0 | 0 - Inf | 0.9998 |
| Cardiovascular disease | 0 | NA - Inf | 0.9999 |
| Aspirin | 0.03 | 0 - Inf | 1.0000 |
| Other antiplatelets | 0 | 0 - Inf | 0.9998 |
| Anticoagulants | 0 | 0 - Inf | 1.0000 |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | 0 | 0 - Inf | 0.9999 |
| Aspirin as analgesics | 7.35 | 0 - Inf | 0.9999 |
| Steroids | 0 | 0 - Inf | 0.9997 |
| Selective serotonin reuptake inhibitors (SSRI) | 0 | 0 - Inf | 0.9999 |
| Proton pump inhibitors (PPI) | 0 | 0 - Inf | 0.9995 |
| HMG-CoA inhibitors (statins) | 6.34 | 0 - Inf | 0.9994 |
Table 5.
Adjusted odds ratios and 95% confidence intervals from multiple logistic regression in cerebral infarction*
| Variables | Adjusted OR | 95% CI | p-value |
|---|---|---|---|
| (Intercept) | 3.649383e+06 | 0.00 - 4.410196e+298 | 0.9989 |
| Gender† | 5.55 | 0.03 - 5.986921e+04 | 0.5902 |
| AgeOp†† | 0.98 | 0.82 - 1.13 | 0.7643 |
| SubGroup 1††† | 7.379513e+10 | 0 - Inf | 0.9989 |
| SubGroup 2††† | 230.78 | 0 - Inf | 0.9999 |
| DAPTG 6†††† | 19.82 | 0.50 - 5050.15 | 0.1653 |
| DAPTG 9†††† | 0 | 0.00 - 1.589189e+189 | 0.9988 |
| DAPTG 12†††† | 0 | 0 - Inf | 0.9990 |
| DAPTG 13†††† | 273 | 3.35 - 2.300476e+05 | 0.0353 |
| Diabetes | 2.55 | 0.04 - 586.27 | 0.6789 |
| Hypertension | 3.082790e+07 | 0.00 - 5.446095e+113 | 0.9974 |
| Cardiovascular disease | 4.05 | 0.01 - 646.67 | 0.5401 |
| Aspirin | 0.03 | 0.00 - 2.16 | 0.1346 |
| Other antiplatelets | 0.03 | 0.00 - 0.34 | 0.0173 |
| Anticoagulants | 0 | NA - Inf | 0.9995 |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | 0 | 0.00 - Inf | 0.9978 |
| Aspirin as analgesics | 0 | 0.00 - 0.00 | 0.9996 |
| Steroids | 0.59 | 0.02 - 15.27 | 0.7478 |
| Selective serotonin reuptake inhibitors (SSRI) | 0 | NA - Inf | 0.9987 |
| Proton pump inhibitors (PPI) | 2.21 | 0.10 - 82.65 | 0.6110 |
| HMG-CoA inhibitors (statins) | 0 | 0 - 1.858872e+262 | 0.9988 |
REFERENCES
1. Bendok BR, Parkinson RJ, Hage ZA, Adel JG, Gounis MJ. The effect of vascular reconstruction device-assisted coiling on packing density, effective neck coverage, and angiographic outcome: an in vitro study. Neurosurgery. 2007 Oct;61(4):835-40; discussion 840-1.

2. Bodily KD, Cloft HJ, Lanzino G, Fiorella DJ, White PM, Kallmes DF. Stent-assisted coiling in acutely ruptured intracranial aneurysms: a qualitative, systematic review of the literature. AJNR Am J Neuroradiol. 2011 Aug;32(7):1232-6.



3. Chalouhi N, Jabbour P, Singhal S, Drueding R, Starke RM, Dalyai RT, et al. Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke. 2013 May;44(5):1348-53.


4. Cho YD, Lee JY, Seo JH, Lee SJ, Kang HS, Kim JE, et al. Does stent implantation improve the result of repeat embolization in recanalized aneurysms? Neurosurgery. 2012 Dec;71(2 Suppl Operative):ons253-9; discussion ons259.


5. García-Rodríguez LA, Gaist D, Morton J, Cookson C, González-Pérez A. Antithrombotic drugs and risk of hemorrhagic stroke in the general population. Neurology. 2013 Aug;81(6):566-74.


6. García Rodríguez LA, Martín-Pérez M, Hennekens CH, Rothwell PM, Lanas A. Bleeding risk with long-term lowdose aspirin: a systematic review of observational studies. PLoS One. 2016 Aug;11(8):e0160046.



7. Goto S, Izumi T, Nishihori M, Imai T, Araki Y, Kanamori F, et al. Antiplatelet therapy discontinuation after stent-assisted coil embolization for intracranial aneurysms: a single-center, long-term, retrospective, observational study. J Neurosurg. 2022 Aug;1-8.

8. Hart RG, Halperin JL, McBride R, Benavente O, Man-SonHing M, Kronmal RA. Aspirin for the primary prevention of stroke and other major vascular events: meta-analysis and hypotheses. Arch Neurol. 2000 Mar;57(3):326-32.


9. He J, Whelton PK, Vu B, Klag MJ. Aspirin and risk of hemorrhagic stroke: a meta-analysis of randomized controlled trials. Jama. 1998 Dec;280(22):1930-5.


10. Hetts SW, Turk A, English JD, Dowd CF, Mocco J, Prestigiacomo C, et al. Stent-assisted coiling versus coiling alone in unruptured intracranial aneurysms in the matrix and platinum science trial: safety, efficacy, and mid-term outcomes. AJNR Am J Neuroradiol. 2014 Apr;35(4):698-705.



11. Hong N, Cho YD, Kim HS, Pang CH, Yoo DH, Kim JE, et al. Is it safe to discontinue antiplatelet medication after stent-assisted coil embolization? If so, when is the best time? J Neuroradiol. 2022 Mar;S0150-9861(22)00105-5.

12. Hwang G, Kim JG, Song KS, Lee YJ, Villavicencio JB, Suroto NS, et al. Delayed ischemic stroke after stent-assisted coil placement in cerebral aneurysm: characteristics and optimal duration of preventative dual antiplatelet therapy. Radiology. 2014 Oct;273(1):194-201.


13. Kim KS, Fraser JF, Grupke S, Cook AM. Management of antiplatelet therapy in patients undergoing neuroendovascular procedures. J Neurosurg. 2018 Oct;129(4):890-905.


14. Kim TG, Yu S. Big data analysis of the risk of intracranial hemorrhage in Korean populations taking low-dose aspirin. J Stroke Cerebrovasc Dis. 2021 Aug;30(8):105917.


15. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-467.


16. McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med. 2006 Aug;119(8):624-38.


17. Mocco J, Fargen KM, Albuquerque FC, Bendok BR, Boulos AS, Carpenter JS, et al. Delayed thrombosis or stenosis following enterprise-assisted stent-coiling: is it safe? Midterm results of the interstate collaboration of enterprise stent coiling. Neurosurgery. 2011 Oct;69(4):908-13; discussion 913-4.



18. Oxley TJ, Dowling RJ, Mitchell PJ, Davis S, Yan B. Antiplatelet resistance and thromboembolic complications in neurointerventional procedures. Front Neurol. 2011 Dec;2:83.



19. Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke. 2010 Jan;41(1):110-5.


- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 3,135 View
- 93 Download
- ORCID iDs
-
Tae Gon Kim

https://orcid.org/0000-0001-6258-6412 - Related articles
-
Hemodynamic Infarction Associated with Coil Embolization of Intracranial Aneurysm.2003 March;5(1)
Stent-assisted Coil Embolization of Cerebral Aneurysms: Review Article.2011 March;13(1)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



