 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 17(4); 2015 > Article |
|
Abstract
Pseudoaneurysms of the superficial temporal artery are rare and may be treated by manual compression, surgical intervention, coil embolization, or percutaneous thrombin injection. We present a novel technique of local ultrasound guided low-profile coil embolization of the superficial temporal artery with both satisfactory cosmetic and surgical results.
Pseudoaneurysms of the superficial temporal artery (STA) are rare but potentially serious vascular lesions. Early diagnosis and treatment is essential to prevent thromboembolism, rupture, or skin necrosis.14)19) STA pseudoaneurysms are most often complications arising from blunt head trauma, however, penetrating head injuries, hair transplantation, and various surgical procedures, including craniotomy and external ventricular drain placement are also documented causes.2)4)8)12) Time to presentation typically ranges from 2-6 weeks.13) Patients most often present with a painless, enlarging, pulsatile mass in the fronto-temporal region, often accompanied by headache or auricular discomfort.19) Definitive diagnosis can be made by duplex ultrasonography, CT angiography, or angiography.16)
Current treatment modalities include open surgical treatment with ligation and excision, endovascular coil embolization, and ultrasound guided percutaneous thrombin injection.5)9)16) Recently Kim et al.6) report 3 cases of STA pseudoaneurysms treated with manual compression alone. Rancic et al.13) reported a novel technique of ultrasound guided afferent and efferent branch ligation through small incisions and percutaneous aspiration of pseudoaneurysm contents. A gold standard for treatment of STA pseudoaneurysms does not exist. We present a treatment modality which resulted in full obliteration of the pseudoaneurysm with prevention of long term cosmetic defect from coil burden or pseudoaneurysm thrombosis.
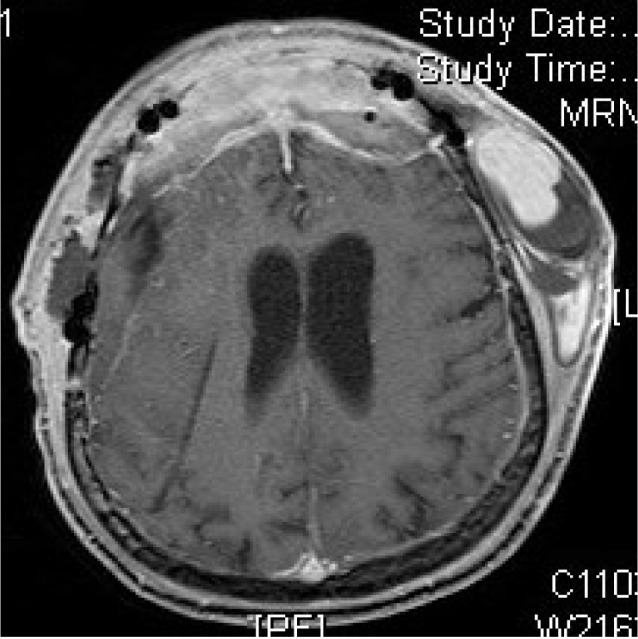
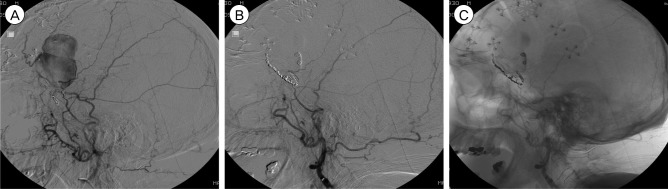
A 78 year-old male underwent bifrontal craniotomy and frontal sinus cranialization with resection of a right sphenoid wing meningioma and right frontal parasagittal meningioma. The patient recovered well and the immediate perioperative period was uncomplicated. Three weeks after surgery he presented with a large pulsatile left temporal mass anterior to the surgical incision site. A contrasted MRI demonstrated a 7.5 × 5 × 2 cm complex hematoma over the left calvarium with flow void concerning for a pseudoaneurysm (Fig. 1). Digital subtraction angiography confirmed STA pseudoaneurysm (Fig. 2).
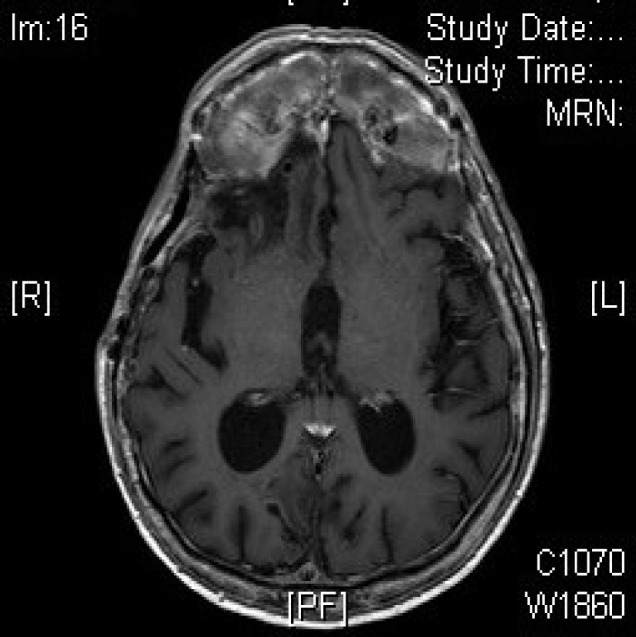
Treatment strategies were discussed in detail with the patient. Thrombin injection was deemed inappropriate due to the large size of the pseudoaneurysm. Catheter coil embolization of the pseudoaneurysm was attempted via right femoral artery access but was unsuccessful due to tortuous parent vessels. With local anesthetic, ultrasound guided access of the STA just proximal to the site of the pseudoaneurysm was then performed. A 4 French catheter was used for access through the scalp distal to the pseudoaneurysm. Thirteen fibered microcoils were delivered sequentially into the STA until the distal and proximal defects were occluded. A post-coil angiogram demonstrated complete obliteration of flow through the pseudoaneurysm (Fig. 3). The contents of the pseudoaneurysm were not aspirated as the decision was made to see if the pseudoaneurysm would decompress naturally. No coils were placed within the pseudoaneurysm in an attempt at obliteration via blockage of both proximal and distal flow. There were no complications of this procedure. At twelve month follow up, MRI demonstrated complete obliteration of the pseudoaneurysm and the patient suffered from no cosmetic sequelae (Fig. 4).
STA pseudoaneurysms are rare vascular lesions that ordinarily occur weeks to months after blunt trauma. Pseudoaneurysms are formed by damage to the arterial wall leading to extravasation of blood and hematoma formation in the surrounding soft tissue.14) The frontal branch of STA is particularly vulnerable since it lies directly above a bony surface and lacks cushioning from overlying muscles.1) Clinical examination reveals an enlarging, pulsatile, painless mass in the distribution of STA with or without a headache. Additionally, STA pseudoaneurysms can be accompanied by regional pain, auditory and visual disturbance and facial palsy.14)15) It is important to treat these lesions due to risk of thromboembolism, rupture, bony erosion, prevent cosmetic disfiguration, and potentially alleviate headache.19)
Current treatment modalities include surgical ligation and resection, endovascular coil embolization, ultrasound guided percutaneous thrombin injection, and conservative surveillance. Surgical ligation and excision is safe, highly effective, and the most common treatment option employed. Once the pseudoaneurysm is located, the afferent and efferent branches of the artery are ligated, followed by excision of the pseudoaneurysm sac. Thomassen et al. and Van Uden et al. reported 128 and 67 cases of STA pseudoaneurysms, respectively, which were successfully treated with surgical excision.18)19) Although highly effective and relatively low risk, complications of surgery include scarring, temporalis muscle wasting, and facial nerve palsy.10)
Recently, alternative treatment options such as endovascular coil embolization and ultrasound guided thrombin injection have gained popularity. In coil embolization, angiography is used to visualize the STA pseudoaneurysm, followed by insertion of platinum microcoils to occlude the lesion.5) Advantages of this method include simultaneous performance of diagnosis and treatment, lack of a surgical scar, decreased risk of scalp infection, and improved recovery time.5) Disadvantages include a 2.8% risk of transient, permanent, or reversible neurologic complications secondary dislocation of an aortic or carotid plaque. Additionally, coil embolization does not address issue of mass effect, and may result in poor cosmesis.16)19)20)
Partap et al.11) described direct injection of thrombin into the pseudoaneurysm under ultrasound guidance. Since then at least five other cases have been successfully treated via this technique, including one case in a pediatric patient.10)18) This method is easy to perform, may be done in the outpatient setting without anesthesia, lacks an incisional scar and has immediate therapeutic benefits for narrow neck pseudoaneurysms less than 4 cm in diameter.11) In addition, there is complete resolution of mass effect created by thrombosis after 2-3 months.11) However, ultrasound guided thrombin injection carries a high rate of risk of recanalization,16) occlusion of the underlying artery, and embolization.10) Teh et al.17) describe a case of ischemia of the scalp and seizure following ultrasound guided thrombin injection, and recommend avoiding this technique when treating pseudoaneurysms of arteries supplying vital end organs.
Gulati et al.3) present the only other report of direct ultrasound guided access to the STA for coil embolization of a STA pseudoaneurysm. After an unsuccessful attempt at manual compression, the pseudoaneurysm was coiled with three one-centimeter coils, leaving a patent STA and completely occluded aneurysm. Complete obliteration was confirmed on ultrasound and by angiography, however, the size of the mass had only decreased by one-third after one month and was not expected to resolve given the mass effect of the coils.3) In our case, the aneurysm was partially thrombosed but still with a large flow void. Given the size of the pseudoaneurysm, the number of coils required for total occlusion, and consequent risk of skin necrosis and poor cosmetic result, the decision was made to perform a low profile coiling of the STA.
We report a case of an iatrogenic STA pseudoaneurysm treated with direct percutaneous ultrasound guided coil embolization of the parent vessel. Post coil angiogram revealed complete occlusion of the pseudoaneurysm. Additionally, there were no recurrences or any cosmetic defects at the one-year follow up. After a review of the literature, Gulati et al.3) describe the only other case using this approach for STA pseudoaneurysm treatment. However, they performed coil embolization of the pseudoaneurysm resulting in a significant coil burden and permanent cosmetic deformity.
A patient's clinical status, aesthetic preferences, and size and chronicity of the pseudoaneurysm are important factors in formulating the right treatment plan for STA pseudoaneurysms.7) We highlight the use of percutaneous ultrasound guided coil embolization as a safe, effective and minimally invasive technique for treating STA pseudoaneurysms. Direct coiling of the STA resulted in a decreased coil burden and diminution of the aneurysm over time. Local, extracranial arterial access avoids the neurologic sequelae sometimes associated with distal access for arteriography. This method is especially useful for poor surgical candidates, patients for whom thrombin injection or catheterization is contraindicated, pseudoaneurysms of significant size and deformity, and for pseudoaneurysms that are difficult to reach with groin or brachial arterial access.
References
1. Ahn HS, Cho BM, Oh SM, Park SH. Traumatic pseudoaneurysm of the superficial temporal artery in a child: a case report. Childs Nerv Syst. 2010 1;26(1):117-120;



2. Angevine PD, Connolly ES Jr. Pseudoaneurysms of the superficial temporal artery secondary to placement of external ventricular drainage catheters. Surg Neurol. 2002 Sep-Oct;58(3-4):258-260;


3. Gulati MS, Gupta H, Sharma S, Kapoor V, Paul S, Berry M. Re: Direct percutaneous coil embolization of a pseudoaneurysm under color Doppler guidance. Cardiovasc Intervent Radiol. 1999 May-Jun;22(3):265-266;



4. Hakan T, Ersahin M, Somay H, Aker F. Pseudoaneurysm of the superficial temporal artery following revision of a middle cerebral artery aneurysm clipping: case report and review of the literature. Turk Neurosurg. 2011 21(3):430-434;


5. Hong JT, Lee SW, Ihn YK, Son BC, Sung JH, Kim IS, et al. Traumatic pseudoaneurysm of the superficial temporal artery treated by endovascular coil embolization. Surg Neurol. 2006 7;66(1):86-88;


6. Kim JH, Jung YJ, Chang CH. Superficial temporal artery pseudoaneurysm treated with manual compression alone. J Cerebrovasc Endovasc Neurosurg. 2015 3;17(1):49-53;



7. Kim SW, Jong Kim E, Sung KY, Kim JT, Kim YH. Treatment protocol of traumatic pseudoaneurysm of the superficial temporal artery. J Craniofac Surg. 2013 1;24(1):295-298;


8. Levisianos I, Sood V. Traumatic aneurysm (pseudoaneurysm) of the superficial temporal artery. Emerg Med J. 2008 4;25(4):239-240;


9. Mann GS, Heran MK. Percutaneous thrombin embolization of a post-traumatic superficial temporal artery pseudoaneurysm. Pediatr Radiol. 2007 6;37(6):578-580;



10. Murphy M, Hughes D, Liaquat I, Edmondson R, Bullock P. Giant traumatic pseudoaneurysm of superficial temporal artery: treatment challenges and case review. Br J Neurosurg. 2006 6;20(3):159-161;


11. Partap VA, Cassoff J, Glikstein R. US-guided percutaneous thrombin injection: a new method of repair of superficial temporal artery pseudoaneurysm. J Vasc Interv Radiol. 2000 4;11(4):461-463;


12. Pourdanesh F, Salehian M, Dehghan P, Dehghani N, Dehghani S. Pseudoaneurysm of the superficial temporal artery following penetrating trauma. J Craniofac Surg. 2013 7;24(4):e334-e337;


13. Rancic A, Pecoraro F, Nigro G, Simon R, Frauenfelder T, Mayer D. Branch ligatures and blood aspiration for post-traumatic superficial temporal artery pseudoaneurysm: surgical technique. Gen Thorac Cardiovasc Surg. 2014 1;62(1):68-70;



14. Roman AA, Arsenault AJ, Jackson KD, Price JM. Novel onset of a posttraumatic superficial temporal artery pseudoaneurysm. Case Rep Emerg Med. 2013 2013:369309




15. Rubio-Palau J, Ferrer-Fuertes A, Garcia-Diez E, Garcia-Linares J, Marti-Pages C, Sieria-Gil R. Traumatic pseudoaneurysm of the superficial temporal artery: a case report and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014 2;117(2):e112-e114;


16. Stapleton CJ, Fusco MR, Thomas AJ, Levy El, Ogilvy CS. Traumatic pseudoaneurysms of the superficial temporal artery: case series, anatomy, and multidisciplinary treatment considerations. J Clin Neurosci. 2014 9;21(9):1529-1532;


17. Teh LG, Sieunarine K. Thrombin injection for repair of pseudoaneurysms: a case for caution. Australas Radiol. 2003 3;47(1):64-66;


18. Thomassen I, Klompenhouwer EG, Willigendael EM, Teijink JA. Treatment of temporal artery pseudoaneurysms. Vascular. 2014 8;22(4):274-279;


Fig. 2
(A) Diagnostic angiogram, lateral view, demonstrating a large STA pseudoaneurysm. (B) Diagnostic angiogram, AP view, demonstrating a large STA pseudoaneurysm.

- TOOLS
-
METRICS

-
- 8 Crossref
- 0 Scopus
- 2,158 View
- 22 Download
- Related articles
-
Endovascular Treatment of Symptomatic Vertebral Artery Dissecting Aneurysms2016 September;18(3)




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



