INTRODUCTION
Cerebellar arteriovenous malformations (AVM) comprise 10-15% of intracranial AVMs. A previous report suggested that the Spetzler-Martin grading scale cannot accurately predict microsurgical outcomes for AVMs located in the cerebellum.2) Lawton et al. described the supplementary grading scale, which accounts for patient age, history of AVM rupture, and compactness of the nidus.1) We report two cases of ruptured cerebellar AVMs treated at our institution in which surgical outcomes showed correlation with the supplementary grade but not with the Spetzler-Martin grade.
CASE REPORTS
Case 1
A 16-year-old female presented with sudden onset headache, nausea, and vomiting followed rapidly by coma. Brain computed tomography (CT) showed a large cerebellar hematoma resulting in tonsillar herniation and obstructive hydrocephalus. CT angiography (CTA) showed a left tentorial AVM measuring 12├Ś8 mm in the middle cerebellar peduncle supplied by the left superior cerebellar artery (SCA) and anterior inferior cerebellar arteries (AICA) and draining into the left transverse and straight sinuses (Fig. 1). The AVM was Spetzler-Martin grade II and supplementary grade I. Due to compression of the brain stem by the hematoma, the patient was taken emergently to the operating room in order to undergo suboccipital craniectomy and AVM resection. No residual nidus was observed on post-operative digital subtraction angiography (DSA). The patient had transient abducens and facial nerve palsies, which had resolved at the time of discharge. At 2-month follow-up, the patient had mild dysmetria and intermittent diplopia but had returned to playing softball.
Case 2
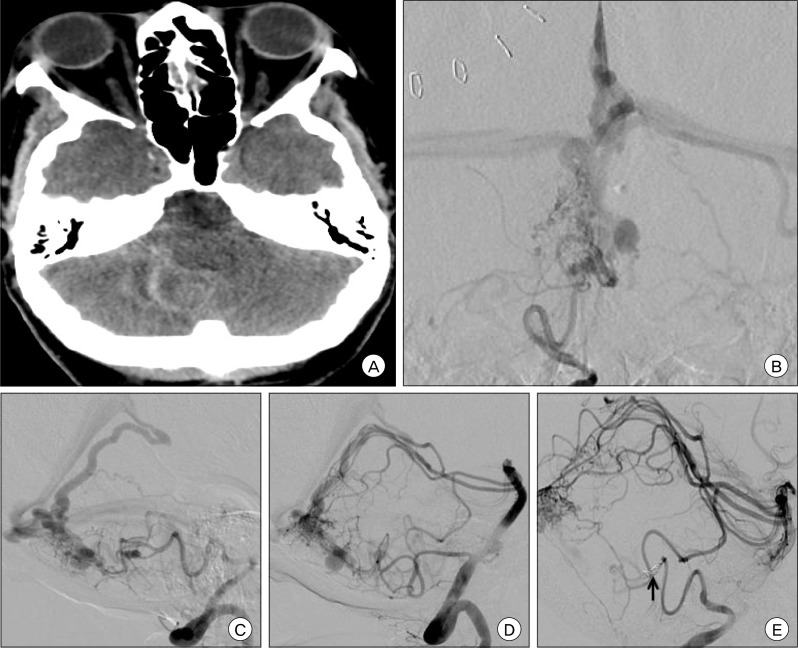
A 59 year-old female was found unresponsive. Brain CT showed a subarachnoid hemorrhage and fourth ventricular hemorrhage resulting in obstructive hydrocephalus necessitating placement of an emergent external ventricular drain. DSA showed a right cerebellar AVM measuring 14├Ś15├Ś13 mm supplied by the bilateral SCAs and posterior inferior cerebellar arteries (PICA) with multiple perinidal aneurysms arising from the feeding right PICA (Fig. 2). The AVM was Spetzler-Martin Grade II and supplementary grade III. Endovascular embolization with polyvinyl alcohol (PVA) and occlusion of the right PICA proximal to the aneurysms was performed prior to surgical resection. The patient subsequently underwent suboccipital craniectomy for AVM resection. The patient's post-operative course was notable for persistent dysphagia requiring placement of a gastrostomy tube, placement of a ventriculoperitoneal shunt, and subclavian thrombus necessitating long-term anticoagulation. The patient was discharged to a nursing home after three weeks of hospitalization.
DISCUSSION
Cerebellar AVMs are a unique subset of intracranial AVMs that present with hemorrhage more frequently than supratentorial AVMs. Due to the relatively small volume of the posterior fossa and their proximity to the brainstem, rupture of cerebellar AVMs may quickly result in devastating neurological consequences. Conversely, neurological decline may be reversed by timely decompression. Neither of the patients described here had operative complications however, they showed significantly different outcomes following resection. The first patient had an eloquent AVM with superficial venous drainage while the second patient had a non-eloquent AVM with deep venous drainage. Based on the Spetzler-Martin grading scale, both AVMs were grade II. However, based on the disparity in age, the first patient was younger than 20 years and the second patient was older than 40 years, the supplementary grades were I and III, respectively.1) This is perhaps an indication of the deteriorating neuroregenerative capability of the brain that accompanies aging.
The utility of grading scales lies in the simplification of complex management decisions into an algorithm for which certain characteristics of patient and lesion may be correlated with treatment outcomes. The Spetzler-Martin grading scale is the most widely used grading system for AVMs.3) Rodriguez-Hernandez et al. hypothesized that the predictive capability of the supplementary grading scale was superior to that of the Spetzler Martin grading scale for assessment of outcomes following microsurgical resection of cerebellar AVMs.2) Deep venous drainage is a better indicator of the depth of the nidus for cerebral AVMs than for cerebellar AVMs. Cerebellar anatomy is altered by AVMs in a different manner than cerebral anatomy such that the supplementary grading scale may be better than the Spetzler-Martin grade for prediction of surgical outcomes. In comparison with ruptured cerebral AVMs, which may be managed conservatively followed by radiosurgery for achievement of obliteration, ruptured cerebellar AVMs may be better treated by surgical resection, especially when the associated hemorrhage results in symptomatic compression of surrounding neural structures.
In conclusion, the surgical risk for cerebellar AVMs may be predicted by either the Spetzler-Martin or supplementary grading scales, although the supplementary scale may show better correlation with outcomes.1-3) However, neither grading system can substitute for experienced clinical and surgical judgment.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






