How to differentiate intracranial atherosclerotic disease or vasospasms after mechanical thrombectomy. Be patient or vasodilator is the secret?
Article information
Abstract
Here we describe a successful mechanical thrombectomy (MT) for acute large vessel occlusion in stroke treatment with one passage (thrombolysis in cerebral infarction, TICI 3). Immediately after the withdrawing of the stent retriever, a narrowing of the middle cerebral artery was diagnosed. The rate of vasospasms during this procedure can be as higher as 41% (range from 6-41%). Here we describe our protocol when a narrowing of the artery is visualized after a stent retriever is withdrawn. A patient presented in our emergency room with National Institute of Health Stroke Scale (NIHSS) of 21, Alberta Stroke Program Early CT Score (ASPECTS) 8, computed tomography angiography revealed occlusion of the M1 segment and MT was indicated. One passage TICI Ⅲ was achieved. After that, the image showed a narrowing of the artery. We present one case of a spasm after stent retriever technique for MT, we injected vasodilator and the artery became normal in a few minutes differentiating between atheromatous stenosis and vasospasm. We present a technical note that can help to make the differentiation of vasospasm or atheromatous disease after MT with the stent retriever technique.
BACKGROUND AND IMPORTANCE
Stroke with large vessel occlusion (LVO) the mechanical thrombectomy (MT) has been the standard treatment after 2015 [2,4,6,7,9]. In almost 85% of the cases in those clinical trials, the stent retriever technique was applied. With the stent apposition in the vascular wall and the friction stimulation during the withdrawing of the device, vasospasm may occur. The image can raise some doubts: is it vasospasm, atheromatous stenosis, dissection or thrombus? This differentiation can, sometimes, be challenging and, in the literature, there are no studies focusing this subject.
CLINICAL PRESENTATION
A patient, in the fifth decade of life, presented in our emergency room with sudden right hemiplegia, Broca aphasia, forced ocular deviation, 3 hours before the hospital admission with a National Institute of Health Stroke Scale (NIHSS) of 21. Computed tomography (CT), Alberta Stroke Program Early CT Score (ASPECT) 8, computed tomography angiography revealed occlusion of the M1 segment of the left middle cerebral artery and the RAPID software (iSchemaView, Menlo Park, CA, USA) calculated a mismatch volume of 61 mL with cerebral blood flow <30% of 10 mL (Fig. 1). IV-tPA was performed 210 min after the onset and MT was indicated. Femoral puncture was done 270 min after the ictus. Under conscious sedation and local anesthesia, the procedure was performed. 9 F short sheath was placed in the right femoral artery, Simmons 5 F diagnostic catheter was used to make an exchanged maneuver and a Cello 9 F balloon guide catheter (Ev3, Irvine, CA, USA) was advanced and positioned in the left internal carotid artery. Digital subtraction angiography demonstrated an occlusion of M1 segment (Fig. 2). Then one Rebar 18 (Ev3, Irvine, CA, USA) microcatheter with a microwire Avigo 0.014 (Ev3, Irvine, CA, USA) was advanced and positioned at M2 segment; a Solitaire FR 4×40 (Ev3, Irvine, CA, USA) (Fig. 2) was advanced and after 5 min was withdrawn (Fig. 2). After one passage Thrombolysis in Cerebral Infarction Ⅲ was achieved 298 min after the onset and 28 min after femoral puncture. Afterwards, the image showed a narrowing of the artery (around 80%). So, we decide to inject 6 mg of milrinone during 10 min and the narrowing image was completely solved (Fig. 2).
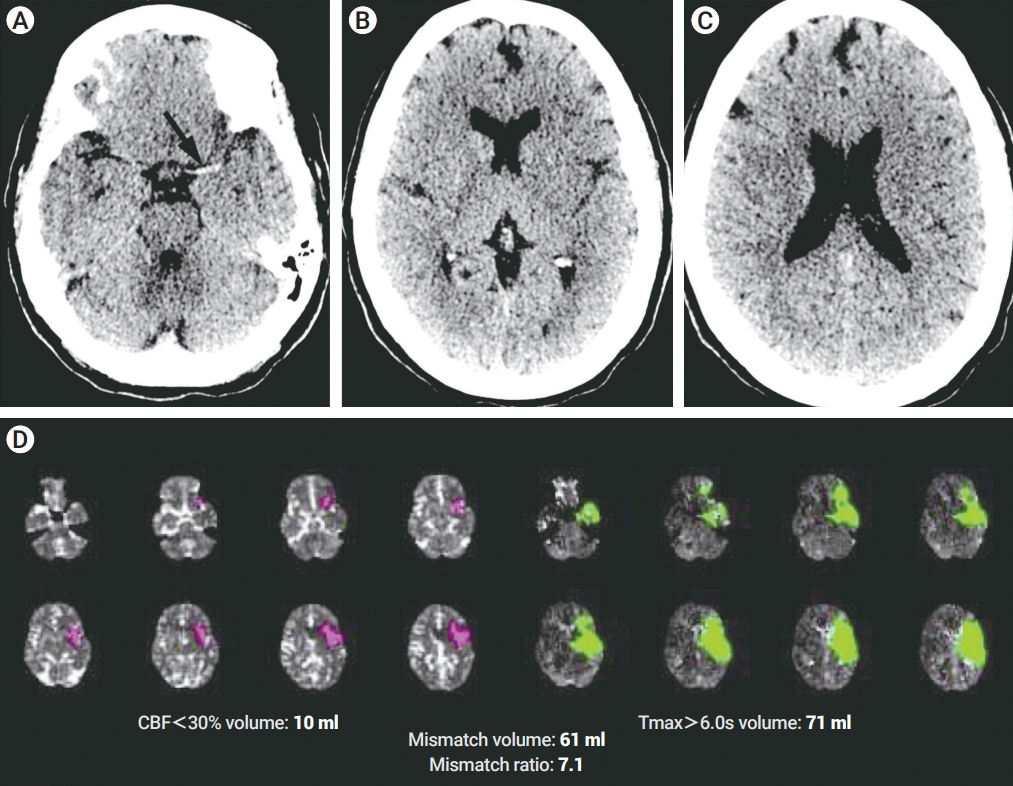
Noncontrast CT. (A) Hyperdense vessel sign on the left (black arrow). (B, C) Early ischemic changes (loss of grey-white matter differentiation). (D) Automated postprocessing of the CTP images (RAPID; iSchemaView, Menlo Park, CA, USA) with CBF <30% of 10 mL; Tmax >6 of 71 mL and mismatch volume: 61 mL. CT, computed tomography; CTP, computed tomography perfusion; CBF, cerebral blood flow.

Left internal carotid artery DSA. (A) First angiographic acquisition confirmed the left M1 segment MCA occlusion (white arrow). (B) The deployment of a Stent retriever–Solitaire FR 4×40 (Ev3, Irvine, CA, USA) (black arrows). (C) First angiographic acquisition after Stent retriever withdrawn with a norrow lesion in the MCA (black arrowhead). (D) Angiographic acquisition after IA 6 mg of milrinone injection throw the balloon guide catheter (Cello 9 F-Ev3, Irvine, CA, USA) with resolution of the vasospasm (white arrowhead). DSA, digital subtraction angiography; MCA, middle cerebral artery.
DISCUSSION
With the large utilization of the MT for LVO strokes, and during the randomized clinical trials almost 85% the stent retriever technique has been applied. Thus, many services use this technique alone or associated with aspiration catheter as first choice to MT. The occurrence of vasospasm becomes more frequent, ranging from 6-41% [1,3,8,10]. The safety of the use of vasodilator during MT has been described by Chalumeau et al. [5].
Another important issue concerning the artery narrowing image: the operator needs to differentiate between vasospasm or atheromatous stenosis. During the procedure it is, sometimes, difficult to know if it is an atheromatous or embolic lesion and the medical decision will be completely different for each of these 2 similar images. Mainly because it prevents the deployment of a Stent, which can be one of the treatments for atheromatous disease but not for vasospasm.
Here we describe our protocol to discern between these 2 images: atheromatous or spasm. After the withdrawing of the stent retriever, we analyze the image. We wait 5 min and another acquisition is done. If the lesion is with the same aspect, we do the injection of vasodilator (in our service we don’t have IV nimodipine and so we use milrinone). During 5-10 min, we inject 6 mg of milrinone and after 5 min another acquisition is done.
CONCLUSIONS
We present one case of a spasm after stent retriever technique for MT. We injected vasodilator and the artery became normal in a few minutes differentiating between atheromatous stenosis and vasospasm. This technical note can help to differentiate of vasospasm or atheromatous disease after MT with the stent retriever technique.
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
