Endovascular occlusion of giant serpentine aneurysm: A case report and literature review
Article information
Abstract
Giant serpentine aneurysms (GSAs) are a rare subgroup of intracranial aneurysms. Separate inflow and outflow flow due to intraluminal thrombosis is the most distinguishing feature of GSAs. In treating these lesions, surgical clipping and ligation were the main treatments in the past, but bypass for revascularisation and endovascular therapies (EVTs) for deconstructive purposes are more prominent today. A 51-years-old male patient presented with headache and mild right hemiparesis. He had a GSA arising from the left fetal type posterior cerebral artery (fPCA) that was out of follow-up for six years. Radiological images revealed midline shifting and mesencephalon compression. We performed endovascular parent artery coil occlusion. The symptoms of the patient improved at the first-month follow-up. Even if there is a mass effect in GSAs, deconstructive EVT is a safe and feasible method for managing these lesions.
INTRODUCTION
Giant serpentine aneurysms (GSAs) were firstly described by Segal and McLaurin in 1977 based on their distinct angiographic features [16]. The GSAs constitute 17.6% of giant aneurysms and less than 0.1% of all intracranial aneurysms [2]. These aneurysms are ≥25 mm, globular, partially thrombosed with a patent, serpiginous vascular channel that courses through the aneurysm. The main feature of GSAs is the existence of separate inflow and outflow tracts and supplying the brain parenchyma with outflow tract [16]. Therefore, unlike saccular variants, GSAs cannot be occluded without ensuring adequate blood supply to the distal territories [1].
The patients have various symptoms, and the most common is the mass effect. The GSAs have a poor prognosis, and they can overgrow if not properly treated. The most common locations of GSAs are the middle cerebral artery (MCA) and posterior circulation [4,15,17].
In the previous decades, surgical clipping was applied to GSAs with or without thrombectomy, and morbidity / mortality rates were reported as 30-35% prior to bypass surgery [1]. Recanalisation techniques have been added to treatment because of the strokes caused by decreased cortical blood flow [4]. Recently, endovascular deconstructive methods aiming to cut off the flow in the aneurysm have become popular [4].
In this paper, we present a GSA that we performed parent artery occlusion by endovascular coiling and discuss 149 GSA cases previously reported in the literature.
CASE REPORT
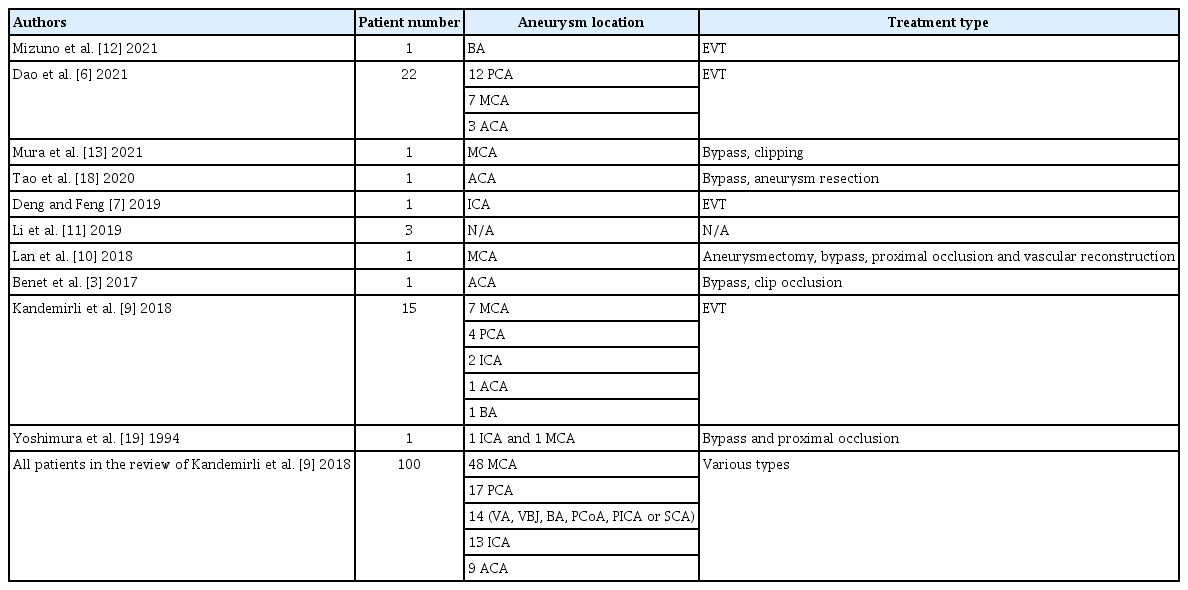
A 51-years-old male was presented with a headache and mild right hemiparesis (4/5 MRC). The patient had a history of untreated GSA. It was diagnosed six years ago (Fig. 1), but he did not accept any surgical or interventional treatment. During this time, he was out of follow-up. Right hemiparesis appeared in the last month. The cranial computed tomography (CT) and contrast-enhanced magnetic resonance imagination (MRI) revealed calcified and thrombosed aneurysm with midline shift (Fig. 2A-F). The diagnostic digital subtraction angiography (DSA) revealed a 59×64 mm GSA arising from fPCA (Fig. 2G, 2H and illustrated in Fig. 3A). Therefore, endovascular transarterial coil embolisation was planned.

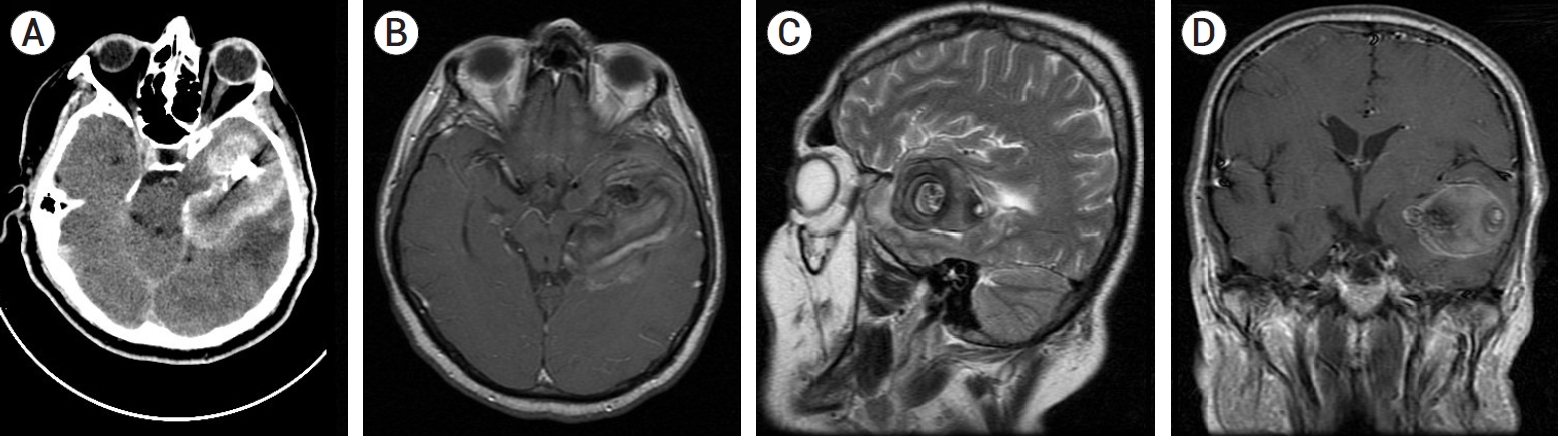
Six years ago, the axial images of contrast-enhanced MRI revealed a thrombosed aneurysm arising from fPCA (A-C). On angiography (D), the serpentine aneurysm that was arising from fPCA appeared. MRI, magnetic resonance imagination; fPCA, fetal posterior cerebral artery.
Serpentine aneurysm with calcified areas and perilesional oedema were observed in axial CT. (A) Contrast-enhanced MRI revealed aneurysm, and mesencephalon compression on axial images (B), perilesional oedema on sagittal images (C, D), and midline shift on coronal (E, F) images. On DSA, anteroposterior (G) and lateral (H) view of an enlarged GSA observed compared to the previous six years. CT, computed tomography; MRI, magnetic resonance imagination; DSA, digital subtraction angiography; GSA, giant serpentine aneurysm.
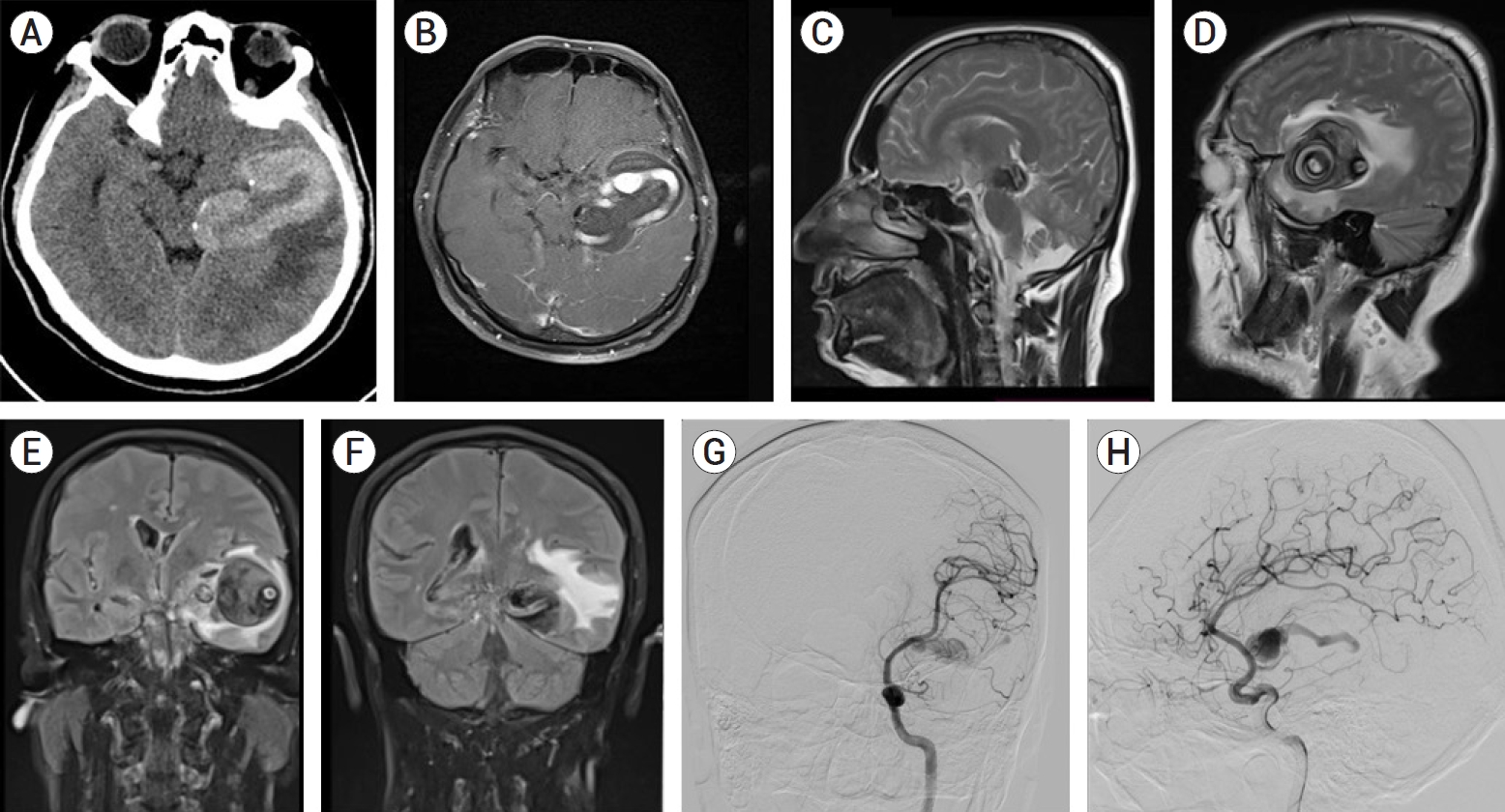
The GSA and intraluminal thrombosis were illustrated in the left temporal region (A). During endovascular therapy, the aneurysm was catheterised with a microwire (B), and imaging was performed with a microcatheter. (C) After the stable coil frame was made (D), it was observed that the aneurysm was totally occluded (E). The fPCA was also patent at the end of the procedure. GSA, giant serpentine aneurysm; fPCA, fetal posterior cerebral artery; PCoA, posterior communicating artery; MCA, middle cerebral artery.
Endovascular treatment
The right femoral artery was punctured under general anaesthesia, and an 11 cm sheath (Arvis, Guangdong, China) was inserted. The systemic heparinisation was performed by intravenous injection of Heparin 5000 unit and repeated 1000 units per hour. The sheath was removed, and a 90 cm 6 Fr long sheath (Heety, Zhejiang Barty Medical Technology, China) was directed to the left internal carotid artery (ICA) up to the high cervical portion, using a Radifocus Guidewire 0.035-inch 180 cm (Terumo, Tokyo, Japan) and 6 Fr Neurobridge 52 catheter 125 cm (Acandis, Pforzheim, Germany) was placed in the petrous segment of the left ICA. A 1.9 Fr microcatheter (APT Medical, Shenzhen, China) was navigated in the left posterior communicating artery (PCoA), proximal to aneurysm, using hybrid micro guidewire (0.014 inches, Balt, CA, USA). (Fig. 3B, 3C) A stable coil frame was made in the spheroid-like space with a 14 mm×47 cm coil (Barricade Complex Frame, Balt, CA, USA). Subsequently, thirteen bare platinum coils (Barricade Complex Frame, Balt, CA, USA) measuring 303 cm were packed into the spheroid-like space (Fig. 3D). At the time, the aneurysm was totally occluded (Fig. 3E). The heparin was neutralised with protamine sulphate (80 mg). Immediate CT has revealed no haemorrhagic or ischemic complications (Fig. 4A). The postoperative period was uneventful. MRI showed no residual filling, regressed mesencephalon compression and perilesional oedema (Fig. 4B-D) at the postoperative first month, and the patient’s symptoms improved.
Literature review
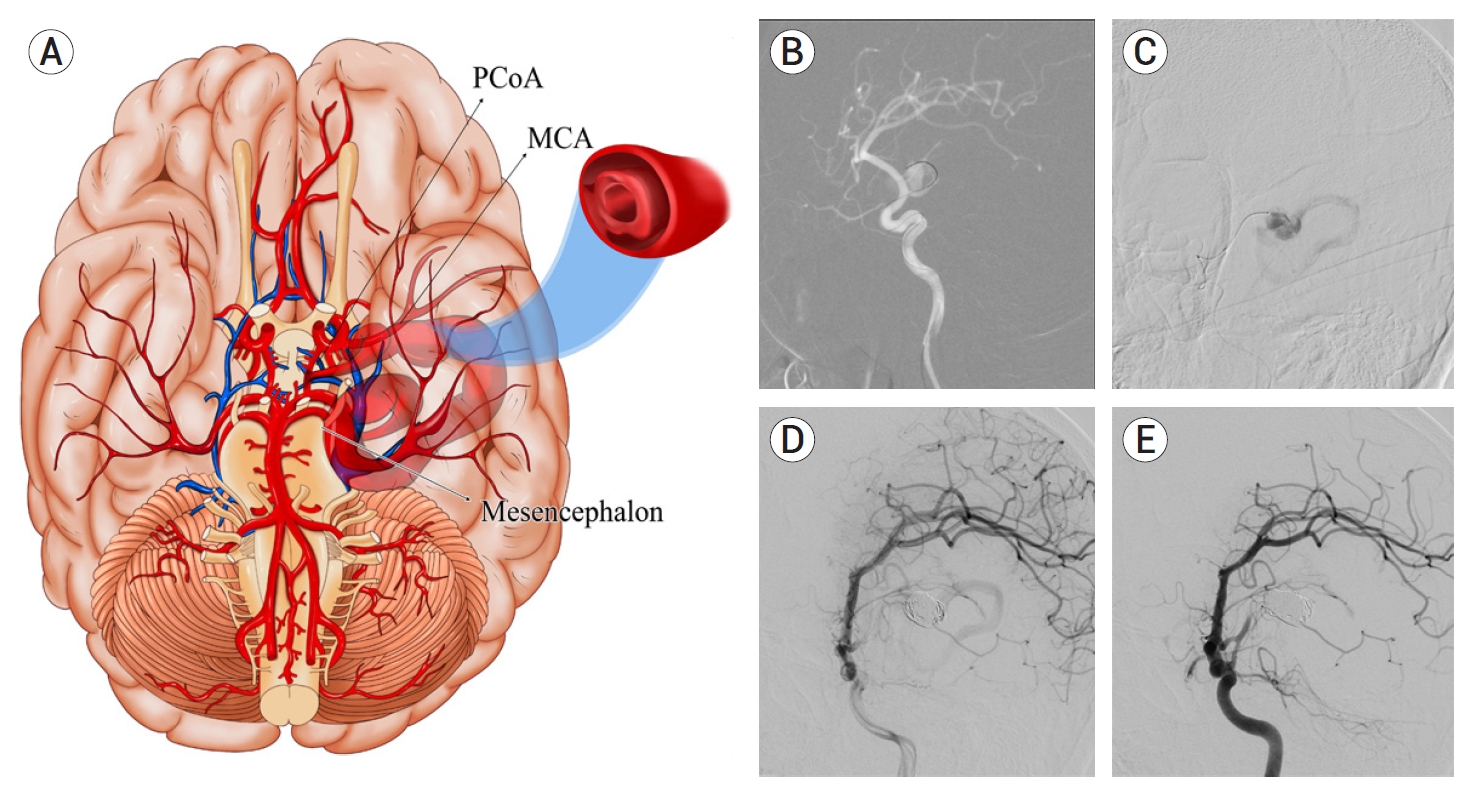
Studies with English abstracts were included in this review, although they were not written in English. The most comprehensive literature review was published by Kandemirli et al. [9] in 2018 and found 100 patients with 101 aneurysms. After this publication, we found 46 more aneurysms (46 patients), including the Kandemirli et al. [9] series. We included an article written in Japanese [19] (1 patient with 2 aneurysms) with an English abstract, ignored by Kandemirli et al. [9]. Thus, the literature has 147 patients with 149 GSAs (Table 1). These aneurysms were most frequently located in MCA (65/149, 43.6%) and followed by PCA (33/149; 22.1%), ICA (17/149, 11.4%), and anterior cerebral artery (ACA) (15/149, 10.1%). The remaining 10.8% were in the vertebral artery (VA), basilar artery (BA), the vertebrobasilar junction (VBJ), superior cerebellar artery (SCA), posterior inferior cerebellar artery (PICA), PCoA, and there was no information about 2% of them.
Of 147 patients, EVT was preferred for 57 (38.8%), surgery for 41 (27.9%), and combined therapy for 9 (6.1%). Spontaneous thrombosis was reported in 4 (2.7%). Conservative treatment was preferred in 6 patients (4.1%), one of which was in locked-in syndrome, and 5 (3.4%) patients accepted as inoperable died. There was not enough information about the treatment modality and outcome of 25 (17%) patients. In addition, four more patients who underwent surgery died, and the total mortality rate was 9/147 (6.1%).
The number of patients whose preoperative neurological examination did not change in the postoperative period was 9 (6.1%). Two of them were intact in the preoperative period. Therefore, surgery was preferred in 7 patients, EVT in 1 patient, and combined therapy in 1 patient.
The number of patients whose preoperative symptoms and neurological examination improved was 81 (55.1%). Of these patients, EVT was preferred for 50, surgery for 23, and combined treatment for eight patients.
The number of patients whose symptoms or neurological examination worsened in the postoperative period was 14 (9.5%). While the treatment modality was EVT in 5 of them who had improvement, the treatment method was surgery in 7 of 9 patients who did not improve, and EVT was in the remaining two.
DISCUSSION
We reported a case of GSA with a mass effect that was successfully treated by endovascular parent artery occlusion. When a GSA is detected, the mass effect puts the surgeon in a dilemma in managing the case. Intraluminal thrombosis, recurrent intraluminal haemorrhage, and intrathrombotic capillary channels are seen in the natural course of these lesions [5]. In a review by Suzuki et al., aneurysmal enlargement because of this process was observed in 12 (30%) of 39 patients over 26 days to 5 years [17]. Similarly, in our patient, both enlargement and serpentinous appearance occurred during the six years he was left without follow-up.
Surgical approaches used in the pre-endovascular era are aneurysm clipping, trapping, wrapping, resection (with or without thrombectomy), and / or parent artery occlusion [4]. With the development of bypass surgery as a revascularisation method, bypass and aneurysm resection have often been applied [4,6,13]. Considering that EVTs have become widespread in the last two decades, it is noticed that they are preferred more often than surgical approaches [6,9]. These approaches are deconstructive type treatments [4,6]. As a combined approach, preoperative embolisation can reduce the bleeding rate during surgical thrombectomy [8]. Regardless of whether the surgical or EVT method is preferred in the treatment, morbidity and mortality are high in any case [1,17].
However, since there are only 149 aneurysms presented in the literature [3,6,7,9-13,18,19, it is impossible to reach a consensus on which method will provide an effective treatment option with low morbidity / mortality. Until the mid-1990s in the literature, the most frequently used methods in the pre-endovascular era were surgical resection, trapping, and bypass at a low rate. During this period, ICA ligation and wrapping methods were also used. In the endovascular era, the most frequently applied method is parent artery occlusion, and the rate of bypass surgery and hybrid approaches has increased compared to the previous period [9]. In current publications, patients who underwent surgery are published as case reports [13,18], while the series [6,9] are generally patients who underwent EVT.
Christiano et al. [4] suggested the following flow in the management of GSAs: CT/CT angiogram and MRI/MRI angiography are applied in the first stage. Subsequently, DSA, which is still the gold standard for diagnosis, is performed. Next, balloon test occlusion or WADA or functional MRI is applied as provocative tests. If neurological deficits develop during these tests, the bypass option is preferred. Proximal/ distal ligation, resection/ reconstruction of the aneurysm, thrombectomy, or carotid ligation can be added to bypass surgery. If neurological deficits do not develop in provocative tests, endovascular occlusion methods (coils, n-Butyl Cyanoacrylate (NBCA) glue, or onyx) are preferred.
The main insufficiencies of EVTs are the inability to reduce the mass effect after the procedure and ischemic complications that may occur if collateral blood supply is insufficient in the distal territories [15]. Although the patient presented in this report had oedema, midline shift, and mesencephalon compression, endovascular deconstructive treatment was preferred. The endovascular occlusion method will lead to the continuation of the mass effect by inducing thrombosis [14]. However, Otsuka et al. [14] discussed that when this mass effect is removed with surgery, the contusion that will occur in the vital structures and the damage to the vascular structures and nerves in the surrounding area will pose a more significant problem than the mass effect. In addition, the spherical mass can prevent the view of the GSA orifice during surgery. Despite the mass effect created by EVT, clinical improvement was observed in 75% of the cases. These facts were decisive in our selection of EVT, although there was a mass effect in our case. Our reason for not performing provocative tests as required by the flow [4] was that the branch from which the aneurysm originates is not suitable for these tests and does not supply any distal territories. Although the vascular structure in the distal of the aneurysm was functional in DSA 6 years ago, this vascular structure was seen to be enlarged in the current DSA and was considered as not functional (Fig. 1D, Fig. 2G, 2H).
CONCLUSIONS
The management of GSAs requires careful evaluation of the patient’s neurological examination, CT / MRI, and DSA findings together. In addition, the mass effect should be considered in the decision-making process. Although the presence of mass effect leads the surgeon to decompressive surgical methods in treatment, deconstructive EVTs are also safe and feasible in managing these lesions.
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.