 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 24(2); 2022 > Article |
|
Abstract
Objective
Cerebral venous thrombosis (CVT) is a rare pathology with life threatening consequences, most of these fatal complications are due to raised intracranial pressure due to venous infarction and cerebral swelling, the purpose of this study is to evaluate the efficiency of decompressive craniectomy for favorable outcome.
Methods
A retrospective analysis of clinical, radiological and surgical data of patients who underwent decompressive craniectomy for CVT in a tertiary referral hospital between the years 2016 through 2020.
Cerebral venous thrombosis (CVT) is one of the most devastating cerebrovascular disorders with 15% mortality rate [3], it accounts for only 0.5% of all strokes [16]. Presentation of such pathology varies vastly among cases, presentation includes headache, visual deterioration, focal neurological deficit and altered conscious level [17]. These non-specific symptoms make diagnosis more challenging, however recent advances and availability of non-invasive vascular imaging made diagnosis more approachable recently [16].
CVT can be predisposed by general pathologies e.g. infection, dehydration, pregnancy, anti-phospholipid syndromes, puerperium and oral contraceptives, several local pathologies can also predispose to CVT e.g. brain tumors, CNS infection, skull base fractures arteriovenous malformations [13,22]. This pathology is rarely encountered above age of 60 years with most commonly affected females between 20 and 35 years, this can be attributed to pregnancy, puerperium and oral contraceptives [1].
Unlike ischemic stroke, CVT is liable to hemorrhagic transformation and subsequently raised intracranial pressure (ICP) [3]. The concept of decompressive craniectomy is well established for cases of ischemic stroke with raised ICP, on the other hand, it’s hypothetically beneficial for all other pathologies with raised ICP and impending herniation as well [19]. CVT’s long term sequela are disabling and considered a cause of permanent disability as well [10]. In this study we present the clinical features and outcome of a series of cases who underwent decompressive craniectomy for raised ICP secondary to CVT. The purpose of this study is to evaluate the outcome of decompressive craniectomy as a line of management for CVT.
Records of patients who underwent decompressive surgery for CVT between 2016 and 2020 in a tertiary referral hospital were reviewed; epidemiological, clinical and radiological data were analyzed, as well as outcome. Institutional agreement is approved, consent is waived due to the retrospective nature of the study.
Non-contrast Computed Tomography (NCCT) brain is the primary surveillance radiology of choice for patients presented with seizures, intractable headache, disturbed conscious level and/or focal neurological deficit. Magnetic resonance imaging (MRI) and MRI venogram (MRV) are indicated when CVT is suspected to evaluate brain parenchyma and venous sinuses respectively (Fig. 1A and B).
Surgical decision was based on both clinical and radiological manifestations of raised ICP, patients who were presented with disturbed conscious level and midline shift more than 5 mm were indicated for surgery immediately, while patients who were presented fully conscious were managed conservatively, surgery was indicated upon deterioration of conscious level. All cases underwent unilateral hemicraniectomy, no cases were indicated for bi-frontal decompression were encountered in this study.
For patients who presented fully conscious, medical treatment is initiated in the form of low molecular weight heparin (therapeutic dose) after initial lumbar puncture and cerebrospinal fluid (CSF) drainage, carbonic anhydrase inhibitor and fluid therapy are given all over the course of treatment.
For patients who underwent decompressive craniectomy, low molecular weight heparin (therapeutic dose) is initiated twelve hours postoperatively after surgery provided that postoperative computed tomography (CT) scans showed no new hemorrhagic events or hematoma expansion, patients are shifted to oral anticoagulant one week after surgery.
Aggressive dehydration is avoided for fear of dehydration induced aggravation of the thrombotic process.
Under general anesthesia, in supine position, a large fronto-tempro-parietal incision is performed followed by generous hemicraniectomy flap (Fig. 1C and D). Pericranium is used to perform duroplasty making the dura lax with no attempt to evacuate the hematoma or excise the infarcted tissue. In cases where vein of Labbe involvement secondary to transverse sinus thrombosis, and the main pathology is temporal swelling, a smaller craniectomy with generous temporal decompression is tailored (Fig. 2).
The study included 7 patients, 2 of them were males (Table 1). Age ranged between 1 and 44 years old, with a mean of 18.14 years. Mean period of symptoms before surgery was 5.86 days which ranged from 1 to 12 days. Headache was a common symptom among all patients except for a one year old patient. Only two patients were presented fully conscious (GCS 15) before they deteriorated and were taken to surgery after 12 and 16 hours respectively. At time of surgery, mean GCS was 8.26 which ranged between 4 and 10. Seizures and motor deficit were presented equally 3/7 each. Predisposing conditions for sinus thrombosis was identifiable in 6/7 patients, 2 infections, 2 oral contraceptives, 1 antiphospholipid disease and 1 dehydration. Unequal pupils was a clinical finding in 2/7 patients at time of surgery.
Five of the seven patients underwent immediate surgery upon presentation with disturbed level of conscious, while 2 patients were initially managed conservatively till surgery was indicated.
The most common involved was the transverse sinus in 6/7 patients, sinus involvement is summarized in table 1. Hemorrhagic transformation of the infarcted brain was found in 5/7 patients, midline shift was found in all patients prior surgery which ranged from 7 and 13 mm, with a mean of 9.29 mm. Only 2 patients showed superficial venous system involvement, both were vein of Labbe.
Outcome in this series was evaluated using Glasgow outcome scale (GOS) as per medical archive due its retrospective nature, GOS is reported upon discharge and 6 months postoperatively.
Good clinical outcome during follow up was achieved for 71.4% (5/7), while one patient suffered permanent disability. We reported one case of mortality (1/7), patient was presented acutely by disturbed conscious level and admitted with GCS 4, unequal pupils which was dilated fixed, age 44 years old.
Mean GOS upon discharge and after 6 months was 3.7 (7 patients) and 4.5 respectively (6 patients), mean follow up period was 11.5 months which ranged from 6 to 18 months.
Six patients who survived underwent cranioplasty within 55 +/- 3 days, one patient suffered flap necrosis and required plastic interference in the form of rotational flap.
CVT is a critical pathology, mortality and morbidity in such pathology may take place via different mechanisms; venous obstruction, CSF flow disruption and most importantly mass effect due to brain swelling and subsequent transtentorial herniation especially when complicated by hemorrhagic transformation [9].
For such a pathology with 8% mortality and 5% disabling morbidity according to the largest CVT series, the question whether or not these patients may benefit from decompression is to be investigated. In one of the largest CVT studies [7], decompressive craniectomy was indicated for only 1.4% of patients which could be attributed to lack of evidence of decompression benefits by the time of the study.
Endovascular thrombolysis and mechanical thrombectomy were studied on a lower scale of case series with discrepant results [11], however better results are found in more recent studies evaluating mechanical thrombectomy due to the new endovascular technologies and peak of experience recently. According to Canhao et al. [4] meta-analysis, 16% of the patients who underwent endovascular local thrombolysis developed intracerebral hemorrhage (ICH), which limited the use of this technique despite achieving 48% recanalization rate. To our understanding, endovascular therapies are not a comparison arm to surgical decompression, as these therapies are primarily designed for the purpose of lumen recanalization which is a treatment for chronic cases or acute cases without malignant CVT since recanalization is not expected to reverse infarction and hemorrhage.
According to the European Federation of Neurologic Societies (EFNS) [6], either low molecular weight heparin (LMWH) or intravenous heparin can be used in cases of CVT, in this series LMWH was used on therapeutic dose which was re-administered 12 hours postoperatively, this protocol is institutional and of no difference to previous studies.
The term malignant CVT was first introduced by Bresson et al. [18] to describe CVT cases with disturbed conscious level which is associated with clinical and/or radiological signs of transtentorial herniation, a term that hypothetically outlines the indications of surgery.
This study population included four adults and three children with female predominance as noted in all previous studies, mean age of patients in our series was 18.14 years which is lower than previous studies which were 39.7 and 35.66 years for Zhang [21] and Aaron [2] respectively, this can be explained by lower number of cases in this study and younger age of our pediatric group; 1, 3 and 4 years old.
In line with our results, the mean duration of symptoms before surgery was 6.47 days for Aaron et al. [2] compared to 5.8 days for this study, while Zhang et al. [21] reported a significantly shorter duration of symptoms by 3.3 days, this can be attributed to the nature of Zhang et al. study which mainly included cases of CVT with hemorrhagic transformation, for those patients course is expected to be faster and more severe, this also explains the lower mean preoperative GCS score, 6.79 for Zhang et al., when compared to 8.2 for this study, and Aaron et al. [2] whose study included only 30% of patients with GCS below 9.
In contrary to previous studies [14], the most commonly affected venous sinus for this study was transverse sinus, while previous studies reported superior sagittal sinus as the most affected sinus. Risk factors for sural sinus thrombosis was identifiable for 8 of the 9 patients, oral contraceptives were the most common predisposing factor for adults (2/4), and infection for pediatric group (2/3), these results matches previously published meta-analysis.
In absence of solid guidelines for decompressive craniectomy in CVT, literature in this topic included small case series. In this series for which mortality rates ranged from 0% to 28.6% [8,15,18,23], one case of mortality is reported (1/9) accounting for 14.2% which is comparable to Zhang et al. (13.8%), this case has met the prognostic criteria of unfavorable by Aaron regarding age (44 years) and preoperative GCS [13]. Although Zhang et al. [21] listed deep venous system involvement as one of the predictive factors of bad prognosis, two patients with vein of Labbe involvement had a good outcome.
Although it appears logic to resect the infarcted brain as a line of mass reduction and hence ICP i.e. internal decompression, it’s known that venous infarction, unlike ischemic infarction, is composed of more edema than necrosis which gives the possibility of reversal of the process [12,20], based on that only external decompression technique was adopted in this study as well as majority of cases in previous studies [2,5,8,21]. Hematoma evacuation was not also attempted, as hemorrhagic transformation of venous infarction pathogenesis leads to diffuse intraparenchymal bleeds which forms small diffuse bleeds rather than a well circumscribed hematoma.
According to previous studies, cases with bi-frontal infarcts due to anterior third superior sagittal sinus thrombosis are less likely to deteriorate and require surgical intervention, on contrary patients with isolated vein of Labbe thrombosis are liable to rapid neurological deterioration due to uncal swelling the consequent transtentorial herniation in absence of aggressive radiological findings which requires thorough clinical consideration [2], none of these two patient subsets were encountered in our study.
GOS was adopted to evaluate outcome in this study, good functional outcome (GOS 5 and 4) was reported in five (71.4%) by the 6th months of follow up, this is in line with Aaron et al. [2] who adopted modified Ranking scale (mRS) with 68% of patients less than 2 mRS after 6 month, also Zhang et al. [21] reported 56.9% good functional outcome, which is slightly less than our results and Aaron’s, this can be due to Zhang et al. focus on hemorrhagic cases only who carry worse outcome.
Limitation of this study includes the low number of cases and absence of comparison to the full CVT population as patients were referred to neurosurgical care only when indicated for surgery. Further larger scale studies are encouraged to solidify and/or add to the current surgical indications.
Decompressive craniectomy is a lifesaving procedure for cases of malignant venous edema to decrease intracranial pressure, survivors are expected to have a good functional outcome without disability in majority of cases, randomized prospective studies should be performed to establish guidelines for early surgical intervention.
Fig. 1.
Twenty-three years old female patient, presented to emergency room with disturbed conscious level and seizures, GCS on presentation was 10. CT brain showed hemorrhagic infarction with mass effect and midline shift of 8 mm (A), MRI with contrast showed filling defect in right transverse sinus (red arrow) (B). Decompressive craniectomy was performed, immediate follow up radiology
showed sufficient decompression and improvement of midline shift (C and D). GCS, Glasgow coma score; CT, computed tomography; MRI, magnetic resonance imaging

Fig. 2.
Three years old male child’s MRI showing welling of the right temporal lobe and herniation (A), MRV showed thrombosis of right transverse sinus and vein of Labbe (B), decompressive craniectomy was performed which was tailored more towards temporal bone, two weeks follow up CT scan showing improvement of midline shift with residual increased CSF tension in subcutaneous collection (C), and the corresponding clinical follow up where patient was fully conscious with no deficit (GOS 5) (D). Six weeks follow up CT scan showing improvement of mass effect and midline shift with resolution of all increased tension signs (E). MRI, magnetic resonance imaging; MRV, MRI venogram; CT, computed tomography; CSF, cerebrospinal fluid; GOS, Glasgow outcome scale
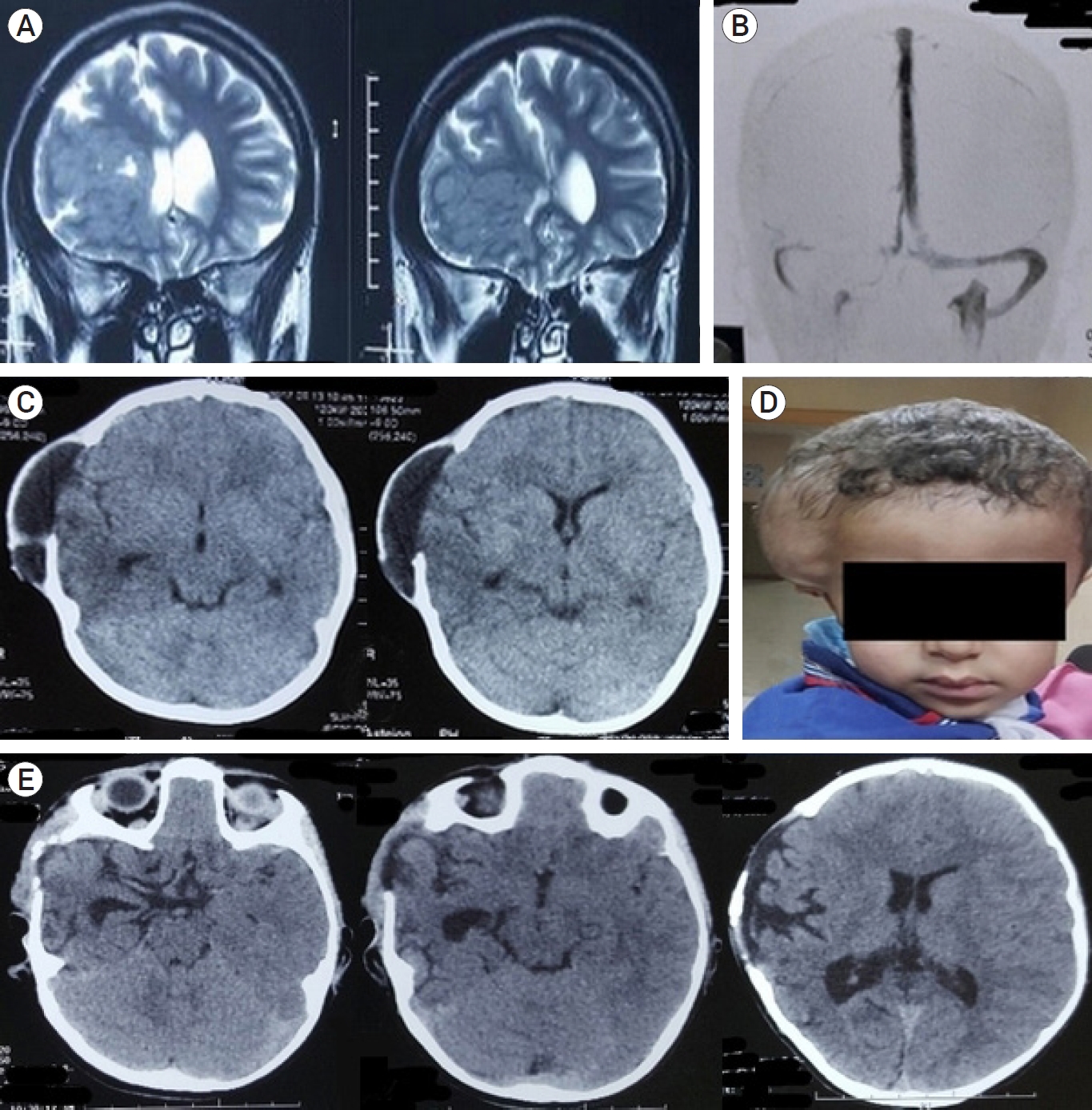
Table 1.
Patients’ data: Clinical and radiological presentation and outcome
REFERENCES
1. Aaron S, Alexander M, Maya T, Mathew V, Goel M, Nair SC, et al. Underlying prothrombotic states in pregnancy associated cerebral venous thrombosis. Neurol India. 2010 58(4):555-9.


2. Aaron S, Alexander M, Moorthy RK, Mani S, Mathew V, Patil AKB, et al. Decompressive craniectomy in cerebral venous thrombosis: A single centre experience. J Neurol Neurosurg Psychiatry. 2013 Sep;84(9):995-1000.


3. Breteau G, Mounier-Vehier F, Godefroy O, Gauvrit JY, Mackowiak-Cordoliani MA, Girot M, et al. Cerebral venous thrombosis: 3-year clinical outcome in 55 consecutive patients. J Neurol. 2003 Jan;250(1):29-35.

4. Canhão P, Falcão F, Ferro JM. Thrombolytics for cerebral sinus thrombosis: A systematic review. Cerebrovascular Diseases. 2003 15(3):159-66.

5. Coutinho JM, Majoie CBLM, Coert BA, Stam J. Decompressive hemicraniectomy in cerebral sinus thrombosis: Consecutive case series and review of the literature. Stroke. 2009 Jun;40(6):2233-5.


6. Einhäupl K, Stam J, Bousser MG, De Bruijn SFTM, Ferro JM, Martinelli I, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients. Eur J Neurol. 2010 Oct;17(10):1229-35.


7. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis: Results of the international study on cerebral vein and dural sinus thrombosis (ISCVT). Stroke. 2004 Mar;35(3):664-70.


8. Ferro JM, Crassard I, Coutinho JM, Canhão P, Barinagarrementeria F, Cucchiara B, et al. Decompressive surgery in cerebrovenous thrombosis: A multicenter registry and a systematic review of individual patient data. Stroke. 2011 Oct;42(10):2825-31.


9. Girot M, Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F, et al. Predictors of outcome in patients with cerebral venous thrombosis and intracerebral hemorrhage. Stroke. 2007 Feb;38(2):337-42.


10. Hiltunen S, Putaala J, Haapaniemi E, Tatlisumak T. Long-term outcome after cerebral venous thrombosis: Analysis of functional and vocational outcome, residual symptoms, and adverse events in 161 patients. J Neurol. 2016 Mar;263(3):477-84.


11. Ilyas A, Chen CJ, Raper DM, Ding D, Buell T, Mastorakos P, et al. Endovascular mechanical thrombectomy for cerebral venous sinus thrombosis: A systematic review. J Neurointerv Surg. 2017 Nov;9(11):1086-92.


12. Keller E, Pangalu A, Fandino J, Könü D, Yonekawa Y. Decompressive craniectomy in severe cerebral venous and dural sinus thrombosis. Acta Neurochir Suppl. 2005 94:177-83.


13. Lee SS, Baek SH, Shin DI. A case of cerebral venous thrombosis as the presenting sign of occult prostate cancer. J Clin Neurol. 2009 Dec;5(4):195-7.



14. Mohamed MWF, Aung SS, Mereddy N, Ramanan SP, Hamid P. Role, effectiveness, and outcome of decompressive craniectomy for cerebral venous and dural sinus thrombosis (CVST): Is surgery really an option? Cureus. 2020 Dec 17 12(12):e12135.



15. Raza E, Shamim MS, Wadiwala MF, Ahmed B, Kamal AK. Decompressive surgery for malignant cerebral venous sinus thrombosis: A retrospective case series from pakistan and comparative literature review. J Stroke Cerebrovasc Dis. 2014 Jan;23(1):e13-22.


16. Saposnik G, Barinagarrementeria F, Brown RD, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011 Apr;42(4):1158-92.


17. Shariff EM, Alhameed M. Multiple cranial neuropathies in cerebral venous sinus thrombosis. Oxf Med Case Reports. 2014 May;2014(2):21-3.



18. Théaudin M, Crassard I, Bresson D, Saliou G, Favrole P, Vahedi K, et al. Should decompressive surgery be performed in malignant cerebral venous thrombosis?: A series of 12 patients. Stroke. 2010 Apr;41(4):727-31.


19. Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: A pooled analysis of three randomised controlled trials. Lancet Neurol. 2007 6(3):215-22.


20. Weber J, Spring A. Unilateral decompressive craniectomy in left transverse and sigmoid sinus thrombosis. Zentralbl Neurochir. 2004 65(3):135-40.


21. Zhang S, Zhao H, Li H, You C, Hui X. Decompressive craniectomy in hemorrhagic cerebral venous thrombosis: Clinicoradiological features and risk factors. J Neurosurg. 2017 Oct;127(4):709-15.


- TOOLS
-
METRICS

-
- 1 Crossref
- 0 Scopus
- 2,510 View
- 76 Download
- ORCID iDs
-
Mohamed M Elsherbini

https://orcid.org/0000-0002-5030-5422 - Related articles
-
Decompressive Craniectomy for Malignant Middle Cerebral Infarction.2009 June;11(2)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



