 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 24(4); 2022 > Article |
|
This article has been corrected. See J Cerebrovasc Endovasc Neurosurg. 2023 Nov 10; 25(4): 485.
Abstract
Vascular anomaly and aneurysmal formation of an anterior communicating artery (ACOM) complex has often been reported. Because of such a complicated relationship between the vascular structure and aneurysms, ACOM aneurysm is one of the most difficult aneurysms to treat among other common anterior circulation aneurysms. We herein report a case of wire perforation of a missed tiny aneurysm arising from the fenestrated A1 segment during the endovascular approach to ACOM aneurysm. Although the fenestration of A1 segment is a rare vascular anomaly, it is likely to accompany saccular type aneurysms in the vicinity of the vascular anomaly. Endovascular treatment for ACOM aneurysm requires more detailed evaluations of the accompanying vascular anomaly and hemodynamics around ACOM to avoid complications.
Vascular anomaly and aneurysmal formation of an anterior communicating artery (ACOM) complex has often been reported [7]. Because of such a complicated relationship between the vascular structure and aneurysms, ACOM aneurysm is one of the most difficult aneurysms to treat among other common anterior circulation aneurysms. Arterial fenestration has an angiographical incidence of 0.3-0.9% and is frequently associated with aneurysms [4]. Some cases of aneurysms arising from the fenestrated A1 segment of the anterior cerebral artery (ACA) have been reported, but the disadvantages of the endovascular procedure have not been well determined [4,6]. We herein report a case of wire perforation of a preoperatively missed tiny aneurysm originating from the proximal bifurcation of the fenestrated A1 segment during the endovascular approach to ACOM aneurysm.
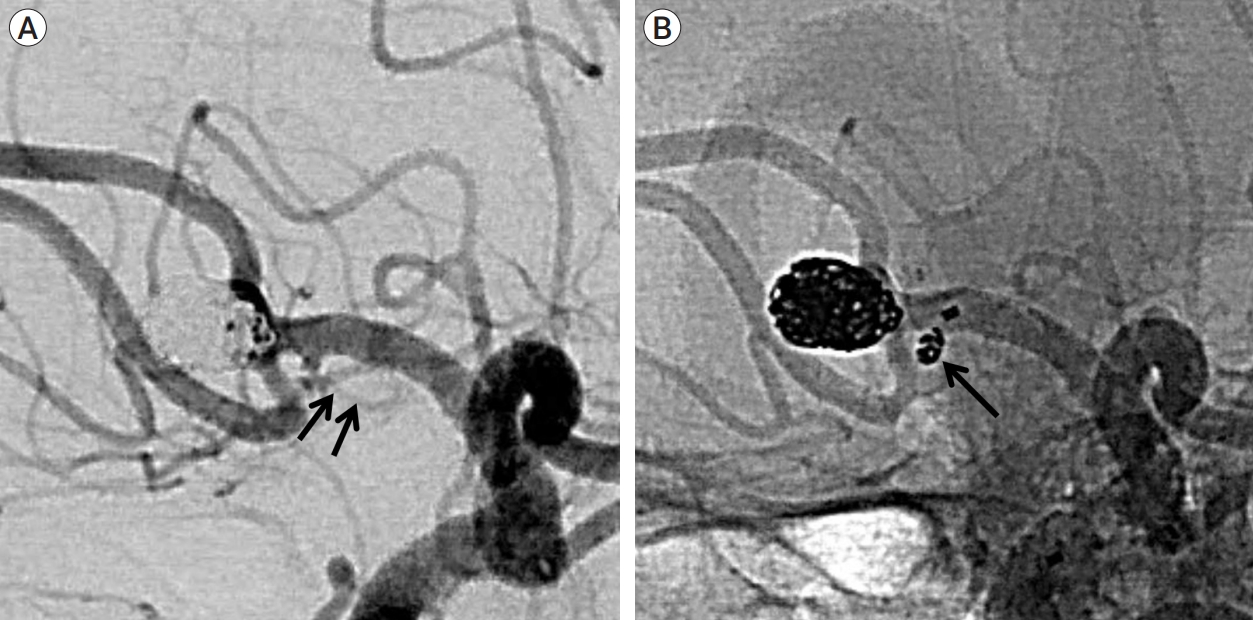
An age 77 female was incidentally diagnosed with an unruptured left ACOM aneurysm. She had been diagnosed with early-staged lung cancer two months ago, and a cerebral aneurysm was discovered in the course of determining the disease’s stage. Cerebral angiography revealed a 7 mm ACOM aneurysm with A1 fenestration (Fig. 1). She underwent endovascular coiling under light sedation. As the microwire passed through the left A1 segment, contrast leakage from mid-A1 segment was identified with a rapid change of her vital signs, suspecting A1 dissection or perforation by the microwire (Fig. 2). To prevent continuous leaking of the contrast material, protamine sulfate was administered for heparin reversal. ACOM aneurysm and injured A1 segment were treated simultaneously with a Solitaire AB stent and coils using a waffle-cone technique (Fig. 3). No bleeding has been observed sine the stent was deployed through the entire A1 segment. Immediately after the procedure, diffuse subarachnoid hemorrhage was observed in brain computed tomography (CT) but she recovered toward relatively good condition. However, a rebleeding that had occurred two hours after the procedure worsened her condition. Repeated cerebral angiography revealed a contrast leakage from the proximal fenestrated A1 segment, immediately embolized using coils (Fig. 4). By careful review of previous angiography, we detected a tiny aneurysm originating from the proximal bifurcation of the fenestrated A1 segment and could speculated that the cause of the intraprocedural bleeding was a wire perforation of a missed aneurysm, not A1 dissection or perforation (Fig. 5). Despite the extraventricular drainage and intensive care, she has not regained consciousness.
Cases of anomaly in the region of the ACOM are numerous, and many studies have reported on ACOM aplasia, duplication of the ACOM or A1 segment, A1 hypoplasia or aplasia, azygous ACA, a median artery of the corpus callosum, and ACA fenestration [7]. Because of such a complicated relationship between the vascular structure and aneurysms, ACOM aneurysm is one of the most difficult aneurysms to treat surgically as well as endovascularly among other common anterior circulation aneurysms.
ACA fenestration has been reported in 0.1-7.2% of dissected autopsy specimens, more frequent than in the distal A1 segment [5]. Embryologically the formation of A1 fenestration could lead to the formation of aneurysms on the fenestrated A1 segment [3]. And, a majority of these aneurysms tend to develop on the proximal end of the fenestrated A1 segment [4]. Hemodynamic stress may induce the formation of aneurysms at the bifurcation, and the development of a fenestrated A1 segment may also be strongly associated with hemodynamic stress at the site of the bifurcation [4]. Thus, it is thought that detailed evaluations of this area are critical before performing the endovascular approach. However, small arteries or tiny aneurysms around the fenestrated A1 segment may not always be identified in digital subtraction angiograms and 3D CT angiograms because of the complexity of cerebral blood flow around them [1]. In our case, the tiny aneurysm around the fenestrated A1 segment was missed preoperatively in radiological examinations. After the coils were filled in the proximal part of the fenestrated A1 segment, the presence of aneurysm became more apparent. Thus, the interventionist should keep this corner area in mind as a weak point and be careful at all times even if an aneurysm in the area was not detected in preoperative evaluations. Additionally, this corner aneurysm is easily accessible when the wire advances the ACOM aneurysm, and it may be easily perforated by wire if it is not easy to control the tension of wire, especially when the angles of internal carotid artery and A1 segment are sharp.
Perforation of a parent artery by a guidewire may have a better prognosis than rupture of a dysplastic vessel or aneurysm [2]. Vascular perforation by a guidewire may result in self-sealing, particularly if it is a puncture rather than a tear [8]. The muscular wall of a normal artery can contract to seal a small perforation [2]. However, anticoagulation during the procedure may disturb the self-sealing of perforated normal artery. Perforation of an aneurysm or dysplastic artery produces a tear in the thin-walled structure. Lacking a muscular wall, flowing blood can enlarge such a tear. Unlike the rupture of the aneurysm, our case showed contrast leakage from mid-A1 segment, so we could suspect A1 perforation or dissection by a microwire. Also, since hemostasis was quickly achieved after stenting, we didn’t consider of other causes of the bleeding at that time. However, because massive re-bleeding had caused us to consider the cause of initial bleeding again, we could detect a tiny aneurysm originating from the proximal bifurcation of the fenestrated A1 segment and could speculate that the cause of that was a wire perforation of a missed that aneurysm, not an A1 perforation or dissection.
Although fenestration of the A1 segment is a rare vascular anomaly, it is likely to accompany saccular type aneurysms in the vicinity of the vascular anomaly. To avoid endovascular procedure-related complications, detailed preoperative evaluations of the anatomical structure and hemodynamics around the fenestration are critical.
ACKNOWLEDGEMENTS
This work was supported by clinical research grant from Pusan National University Hospital in 2021.
Fig. 1.
Subtracted (A) and 3D (B) images of left ICA angiography showing a 7 mm ACOM aneurysm with ACOM fenestration (arrows). ICA, internal carotid artery; ACOM, anterior communicating artery
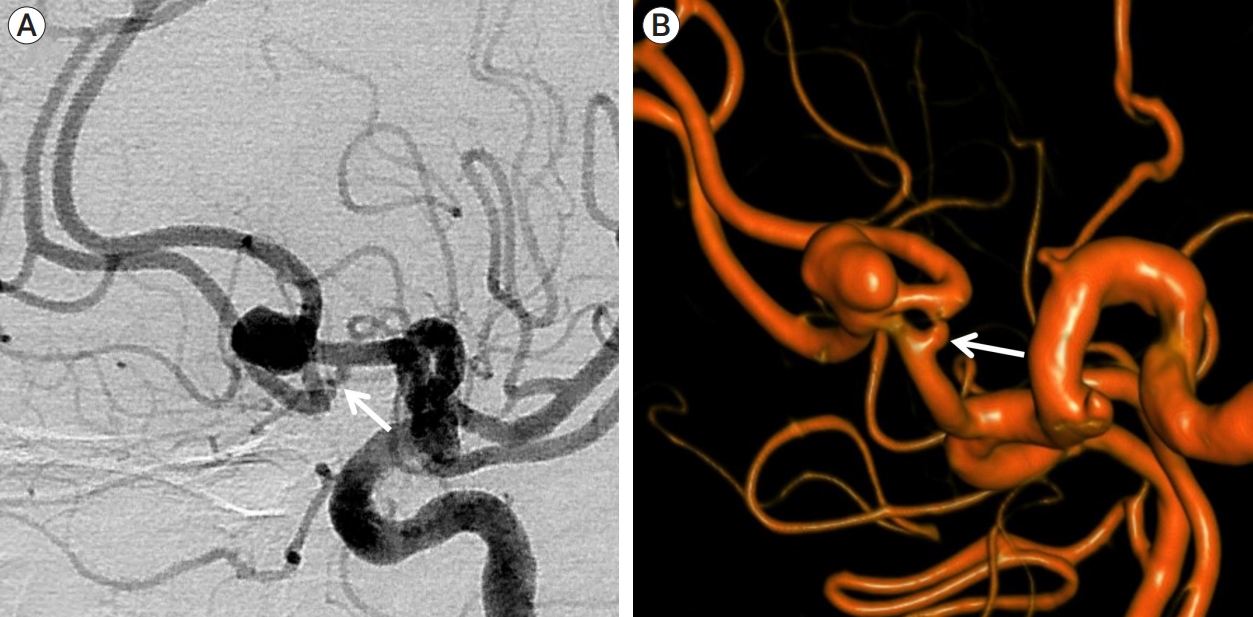
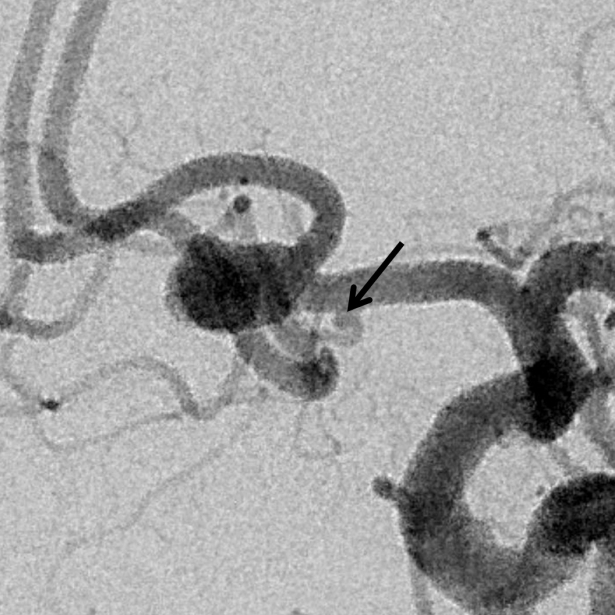
Fig. 2.
Leak of contrast agent surrounding mid A1 indicates intraprocedural bleeding, suspecting A1 dissection by microwire.
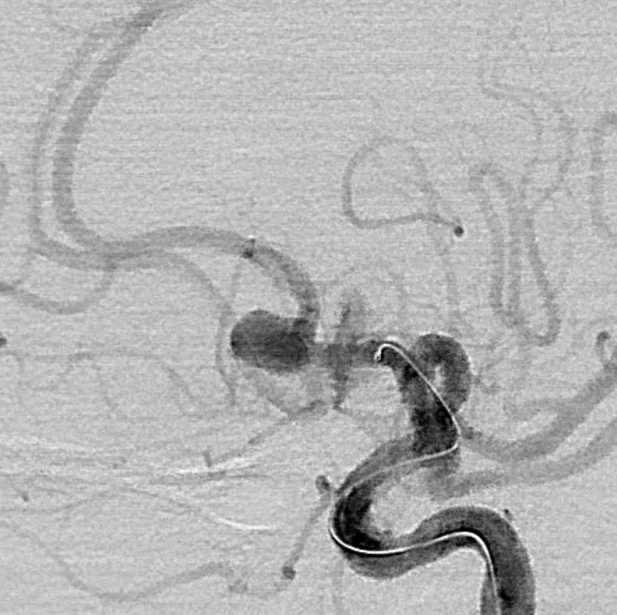
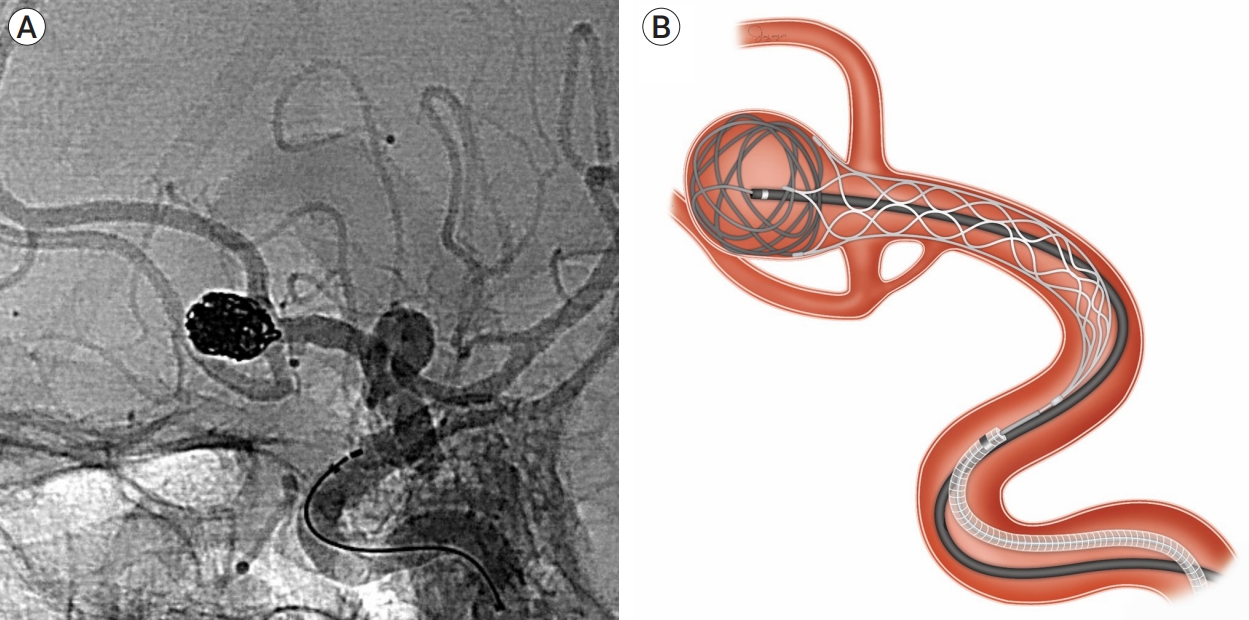
Fig. 3.
Unsubtracted image (A) acquired immediately after stent-assisted coiling using the waffle-cone technique (B) shows no more leak of contrast agent with complete aneurysm occlusion.
REFERENCES
1. de Gast AN, van Rooij WJ, Sluzewski M. Fenestrations of the anterior communicating artery: incidence on 3D angiography and relationship to aneurysms. AJNR Am J Neuroradiol. 2008 Feb;29(2):296-8.



2. Halbach VV, Higashida RT, Dowd CF, Barnwell SL, Hieshima GB. Management of vascular perforations that occur during neurointerventional procedures. AJNR Am J Neuroradiol. 1991 Mar-Apr;12(2):319-27.


3. Ihara S, Uemura K, Tsukada A, Yanaka K, Nose T. Aneurysm and fenestration of the azygos anterior cerebral artery: case report. Neurol Med Chir (Tokyo). 2003 May;43(5):246-9.


4. Iwabuchi N, Saito A, Fujimoto K, Nakamura T, Sasaki T. Unruptured saccular aneurysm arising from the fenestrated A1 segment of the anterior cerebral artery: report of 2 cases. Case Rep Neurol. 2018 Jun;10(2):140-9.




5. Kachhara R, Nair S, Gupta AK. Fenestration of the proximal anterior cerebral artery (A1) with aneurysm manifesting as subarachnoid hemorrhage: case report. Neurol Med Chir (Tokyo). 1998 Jul;38(7):409-12.


6. Kwon WK, Park KJ, Park DH, Kang SH. Ruptured saccular aneurysm arising from fenestrated proximal anterior cerebral artery: case report and literature review. J Korean Neurosurg Soc. 2013 May;53(5):293-6.



- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,612 View
- 44 Download
- ORCID iDs
-
Jun Kyeung Ko

https://orcid.org/0000-0002-5652-7659 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



