Safety of middle meningeal artery embolization for treatment of subdural hematoma: A nationwide propensity score matched analysis
Article information
Abstract
Objective
Middle meningeal artery embolization (MMAe) has burgeoned as a treatment for chronic subdural hematoma (cSDH). This study evaluates the safety and short-term outcomes of MMAe patients relative to traditional treatment approaches.
Methods
In this retrospective large database study, adult patients in the National Inpatient Sample from 2012-2019 with a diagnosis of cSDH were identified. Cost of admission, length of stay (LOS), discharge disposition, and complications were analyzed. Propensity score matching (PSM) was utilized.
Results
A total of 123,350 patients with cSDH were identified: 63,450 without intervention, 59,435 surgery only, 295 MMAe only, and 170 surgery plus MMAe. On PSM analysis, MMAe did not increase the risk of inpatient complications or prolong the length of stay compared to conservative management (p>0.05); MMAe had higher cost ($31,170 vs. $10,768, p<0.001) than conservative management, and a lower rate of nonroutine discharge (53.8% vs. 64.3%, p=0.024). Compared to surgery, MMAe had shorter LOS (5 vs. 7 days, p<0.001), and lower rates of neurological complications (2.7% vs. 7.1%, p=0.029) and nonroutine discharge (53.8% vs. 71.7%, p<0.001). There was no significant difference in cost (p>0.05).
Conclusions
MMAe had similar LOS and decreased odds of adverse discharge with a modest cost increase compared to conservative management. There was no difference in inpatient complications. Compared to surgery, MMAe treatment was associated with decreased LOS and rates of neurological complications and nonroutine discharge. This nationwide analysis supports the safety of MMAe to treat cSDH.
INTRODUCTION
Chronic subdural hematoma (cSDH) is one of the most common neurosurgical pathologies worldwide. Moreover, cSDH disproportionately affects the elderly population and its incidence is projected to increase from 10.35 to 17.6 per 100,000 in the general population by 2030 [3]. The pathophysiology of cSDH is thought to involve bleeding of the bridging veins as they cross through the border cell layer of the dura mater [15]. Hematomas can accumulate asymptomatically until clinical symptoms and signs such as headaches, nausea, seizure, or neurological deficits develop [20]. Trauma history and antiplatelet use have been identified as risk factors for cSDH [2,17].
The traditional management of cSDH includes surgical and nonsurgical interventions. Surgical approaches utilize craniotomy or burr holes for hematoma evacuation. However, these procedures pose some risk of reoperation, unfavorable functional outcomes, and even mortality, which is likely impacted by the advanced age of many cSDH patients [7,12,13,16,17]. Nonsurgical strategies include observation, steroids, atorvastatin, tranexamic acid, and angiotensin-converting enzyme inhibitors, although data on their efficacy are mixed [8].
Enlargement of the middle meningeal artery (MMA) and associated vasculopathies have been implicated in the pathophysiology of cSDH by magnetic resonance angiography [19]. Recently, MMA embolization (MMAe) has grown as both an adjunct to surgery as well as a prophylactic treatment to prevent expansion of cSDH and facilitate reabsorption [4,10,14]. Studies have demonstrated that MMAe has a low complication rate and is safe for elderly patients [4,10].
However, due to the relatively recent implementation of MMAe on a national scale, there are few studies examining rates of adverse outcomes compared to traditional treatment strategies. Moreover, there is potential for selection bias in single-institution studies, as utilization may reflect individual surgeon preferences. In this study, we use the National Inpatient Sample (NIS) to compare in-hospital outcomes of SDH patients treated with conservative management, MMAe, or surgery.
MATERIALS AND METHODS
Data source
The NIS, developed by the Healthcare Cost and Utilization Project (HCUP), is the largest all-payer healthcare database in the United States [1]. HCUP provides survey weights to calculate national estimates and temporal trends for inpatient admissions. Due to public availability of the database, institutional review board approval was not necessary. Patient information in the NIS is de-identified so that patient consent is not required.
NIS admissions between 2012-2019 were identified by International Classification of Diseases, Ninth and Tenth Revision, Clinical Modification (ICD-9-CM and ICD-10-CM) and Procedure Coding System (PCS). Inclusion criteria included age ≥18 years and a diagnosis of SDH (ICD-9 432.1, 852.2, 852.3; ICD-10 I62.00-I62.03, S065*). Treatment with MMAe (ICD-9 39.72, 39.75, 39.76; ICD-10 03LG, 03LM, 03LN) or surgery (using previously published ICD-9 and 10 codes) was identified [12]. Patients were excluded if they had diagnoses or received treatment for aneurysms, neoplasms, precerebral arteriopathies, or dissections [4]. MMAe admissions were individually reviewed to ensure the suitability of their inclusion.
Patient characteristics
Patient characteristics included age, sex, race, All Patient Refined Diagnosis Related Groups (APR-DRG) illness severity and mortality risk scores, long-term use of anticoagulant therapy, coagulopathy, chronic kidney disease, and Elixhauser comorbidity index [6].
Outcomes of interest
Outcomes studied included cost of admission, hospital length of stay (LOS), nonroutine discharge disposition (destination other than home), and complications. Neurological complications included intraoperative nervous system complications, ischemic or hemorrhagic sequelae, facial weakness, and vision loss/blindness. Seizures were analyzed but not classified as a complication due to the difficulty in identifying preexisting seizure conditions versus new postoperative seizures based on ICD codes. Complications were defined by presence of at least one of the following: neurological, respiratory, thromboembolic, cardiac, infectious, or renal.
Statistical analysis
All analyses were completed within complex samples functions, accounting for NIS stratification and weighting in accordance with HCUP guidelines [11]. Descriptive statistics were performed for baseline analyses of demographic and clinical data. Univariable analysis of continuous variables was completed using independent samples t-tests or ANOVA and Wilcoxon rank-sum tests for parametric and nonparametric distributions, respectively. Chi-squared tests were used for categorical variables. Propensity score matching (PSM) was performed to reduce potential sampling bias between cSDH patients who received no intervention versus those who underwent MMAe only; patients who underwent both MMAe and surgery were excluded. Propensity scores were calculated based on the probability of undergoing MMAe using multivariable logistic regression in which patient and hospital characteristics were used as covariates. Separate PSM analyses were performed for MMAe versus conservative management, and MMAe versus surgery. Patients were matched 1:1 using the nearest neighbor method without replacement and a caliper of 0.2 times the standard deviation of the propensity scores. Analyses were performed using Stata version 17.0 (StataCorp LP, USA).
RESULTS
Patient characteristics
A total of 227,116 SDH admissions met inclusion criteria (Table 1). Of these, 381 (0.17%) patients underwent MMAe (64.3% MMAe only, 35.7% MMAe plus surgery). There was a trend toward lower age for patients undergoing MMAe only compared to no-intervention (67.1 vs. 69.4 years, p=0.057). MMAe patients had higher Elixhauser comorbidity indices (p<0.001), were more likely to have elective admissions (13.9 vs. 7.5%, p<0.001), treatment at large hospitals (75.9 vs. 64.6%, p=0.001), teaching hospitals (96.3 vs. 78.2, p<0.001), and hospitals located in the Northeast (36.7 vs. 18.3%, p<0.001). Race, history of coagulopathy or long-term anticoagulation, and chronic kidney disease did not differ between groups (p>0.05). MMAe patients were less likely to have a history of trauma (58 vs. 76.7%, <0.001).
PSM analysis: MMAe vs. no intervention
PSM was performed to account for potential biases in patient treatment groups. MMAe patients had no difference in complications or LOS compared to no-intervention patients (Table 2), but higher cost ($31,170 vs. $10,768, p<0.001) and lower rate of nonroutine discharge (53.8% vs. 64.3%, p=0.024).

Demographic and clinical characteristics of propensity score matched patients treated with MMAe versus conservative management. Univariable comparisons were completed using t-tests and Wilcoxon rank-sum tests for continuous variables and chi-squared tests for categorical variables. NR=Not reported due to n ≤10.
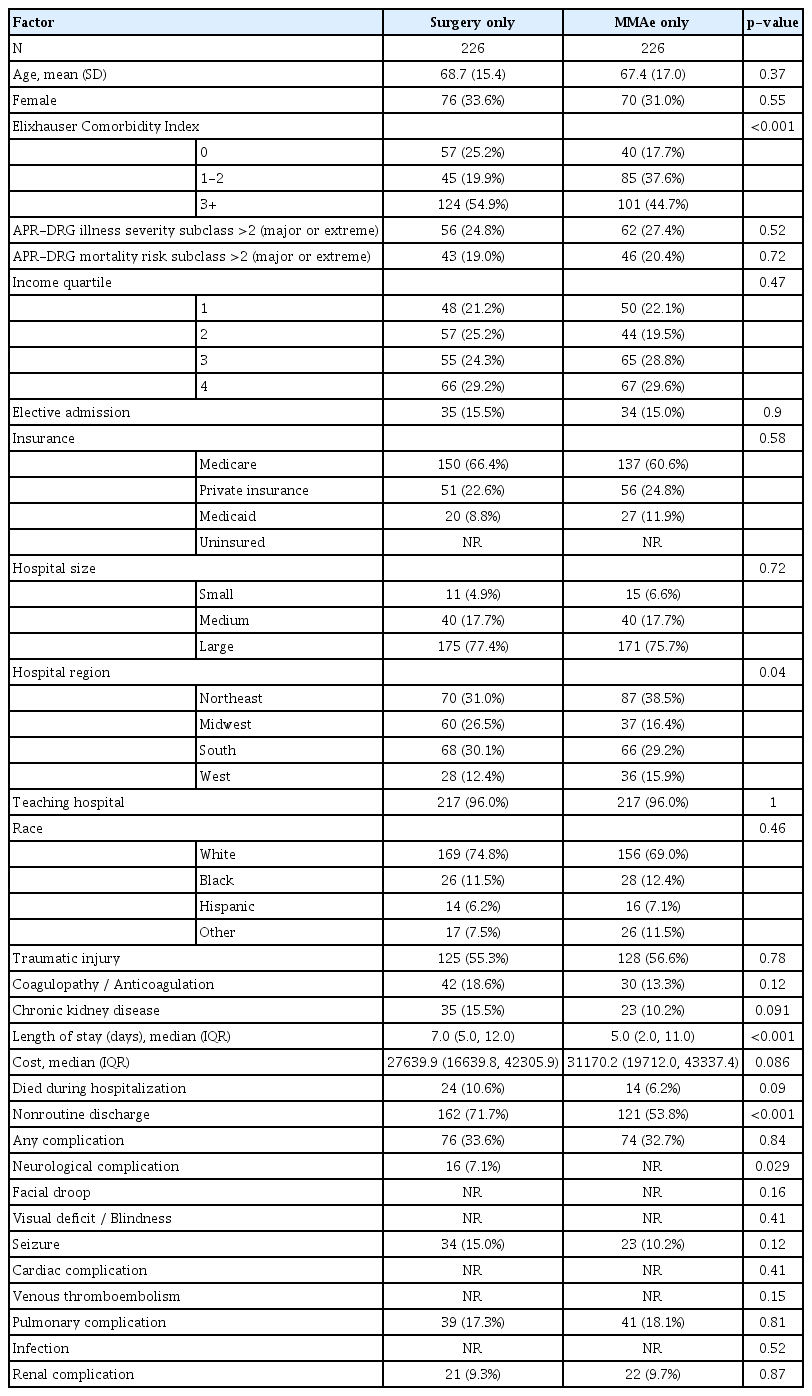
PSM analysis: MMAe vs. surgery
PSM was also completed for MMAe versus surgery (Table 3). MMAe patients had shorter median LOS (5 vs. 7 days, p<0.001), and lower rates of neurological complications (2.7% vs. 7.1%, p=0.029) and nonroutine discharge (53.8% vs. 71.7%, p<0.001). There was a trend towards increased cost of MMAe relative to surgery ($31,170 vs. $27,639, p=0.086) that did not meet statistical significance.
DISCUSSION
MMAe has rapidly become a component of cSDH treatment despite a relative paucity of literature on its safety on a national scale. Most single-institution studies on MMAe for cSDH are relatively small compared to the patient cohort available in the NIS [4,10,14]. Furthermore, the thousands of cSDH admissions in the NIS allowed for propensity score matching on several different patient and hospital factors. In this study, we utilized the NIS to examine the safety of MMA embolization for treatment of cSDH in comparison to surgical and nonsurgical management.
Our data support the safety of MMAe as a treatment modality for cSDH. On PSM analysis, MMAe had a significant decrease in nonroutine discharge, LOS, and neurologic complications compared to surgery. While MMAe is generally not considered an alternative to surgical evacuation for cSDH that meet operative criteria, there may be specific situations in which a comparison of their safety is relevant. For example, patients on anticoagulation who potentially meet operative criteria but have a high risk of stroke if anticoagulation is held for surgery can be good candidates for MMAe as an initial treatment. MMAe does not require patients to pause anticoagulant or antiplatelet medications. Similarly, it has been demonstrated that MMAe is safe for patients of advanced age [5]. Therefore, MMAe may be a favorable treatment strategy in elderly patients for whom surgical evacuation could lead to prolonged recovery and increased risk of further complications.
We found that there was a lower likelihood of neurologic complications with MMAe compared to surgical intervention, which is expected given the minimally invasive nature of MMAe. The significantly shorter LOS and decreased inpatient mortality supports the safety MMAe relative to surgery. Although potential complications of MMAe such as aphasia, seizure, facial palsy, and stroke have been described in the literature, they have a low incidence [9,10]. In a study of 121 patients, the occurrence rate of any adverse event was 2.5% [10]. These low complication rates are comparable to conventional treatments [18]. In our analysis, we found that the rate of neurological complications was significantly lower for MMAe relative to surgical intervention.
We believe there are many cSDH patients that do not meet operative criteria and could be considered candidates for MMAe. As the adoption of MMAe grows, differences in treatment philosophies as well as availability of a neuroendovascular service may influence whether MMAe is offered instead of conservative management. We sought to determine if patients face increased risk of complication or other adverse outcomes with MMAe. Our analysis revealed that MMAe is associated with increased cost of admission but no difference in LOS or complications, and decreased odds of nonroutine discharge disposition. The rates of neurological complications between MMAe and conservative management were both below 3%. These findings suggest that the safety of MMAe is comparable to that of conservative management. These results were consistent with a meta-analysis which found no difference in in-hospital adverse event rates between cSDH patients treated with MMAe or no intervention [9]. This has significant implications for counseling patients on the safety of this procedure as well as expectations regarding LOS. In the appropriate clinical context, MMAe may be considered as an elective, outpatient procedure for cSDH patients.
Recent studies also support the efficacy of MMAe to treat cSDH. A retrospective cohort study from Joyce et al. found that 94% of their embolization procedures to treat cSDH resulted in stable to improved status at follow-up [10]. Additionally, MMAe shows promise in long-term outcomes. A meta-analysis found a significant reduction in cSDH recurrence and rates of surgical rescue in patients treated with MMAe compared to conservative management [9]. MMAe appears to show robust efficacy, however, many of the studies are relatively limited to smaller sample sizes or indirect methods of comparing cohorts. More robust studies are needed to further support the implementation of MMAe for short-term and long-term stabilization or improvement of cSDHs in patients.
Limitations
Limitations of this study include biases in patient selection, as utilization of MMAe may vary between interventionalists, institutions, and geographic regions. While we utilized PSM to reduce the effects of these biases, a prospective multicenter trial would provide a higher level of evidence. There are numerous limitations to the NIS database, including its cross-sectional design without post-discharge outcome data, lack of granularity regarding SDH size, laterality, or chronicity, and the use of billing codes for both diagnoses and procedures. Furthermore, large databases such as the NIS, are subject to coding biases, which may be of greater concern in relatively new procedures [21]. Thus, there may be underrepresentation of complications that were not captured with billing codes. Previous procedures cannot be identified, so it is possible some MMAe patients had surgical evacuation completed on prior encounters. Moreover, the NIS does not temporally order diagnosis codes with procedures, which can make it challenging to differentiate baseline deficits from new post-procedure deficits.
CONCLUSIONS
MMAe continues to grow in popularity in the treatment of cSDH. To our knowledge, this is the largest propensity score matched study comparing MMAe safety to surgical and conservative management. We found that MMAe has a minimal complication profile and is not associated with an increased risk of short-term adverse outcomes compared to conservative management. This work supports the safety of MMAe as an alternative to conservative management for cSDH that don’t require surgical intervention.
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.