Ventriculoperitoneal Shunt in a Patient with Ruptured Blister Aneurysm Treated with Pipeline Embolization Device
Article information
Abstract
Cerebral spinal fluid (CSF) diversion is frequently required in patients with aneurysmal subarachnoid hemorrhage who develop subsequent hydrocephalus. Procedures such as external ventricular drain (EVD) and ventriculoperitoneal shunt (VPS) usually carry a very low rate of complications. However, as flow diverting stents such as Pipeline Embolization Device (PED) become more widely available, flow diverters are being used in treatment of some ruptured complex aneurysms. EVD and VPS placement in the setting of dual antiplatelet therapy (DAT) in these patients are associated with a significant risk of intracranial hemorrhage. We describe a management strategy and surgical technique that can minimize hemorrhagic complications associated with VPS in patients on DAT after treatment with flow diverting stents.
INTRODUCTION
Tremendous strides in neuroendovascular technology have been achieved in the last decade, with the most recent advancement being the flow diverting stents such as Pipeline Embolization Device (PED; ev3/Covidien, Irvine, CA, USA). Flow diverting stents are becoming an increasingly important and widely utilized tool in the treatment of complex cerebral aneurysms. Endovascular treatment of blister or fusiform aneurysms using flow diverters is becoming increasingly popular because open surgical approaches for these lesions are often technically challenging and are associated with significant surgical morbidity. Flow diverting stents have a delayed onset of action in inducing aneurysm thrombosis and universally require dual antiplatelet therapy (DAT), thus their use has been largely limited to treatment of unruptured aneurysms. However, several authors have recently reported good clinical outcome and acceptable morbidity/mortality using flow diverters for treatment of ruptured complex aneurysms.2)4)7)9) Based on these preliminary evidences, flow diverters may a treatment option in selected patients with ruptured complex cerebral aneurysms. One challenging issue with use of flow diverters for ruptured cases, however, is the need for cerebral spinal fluid (CSF) diversion in the setting of DAT. As reported in several studies, hemorrhagic complications associated with external ventricular drain (EVD) or ventriculoperitoneal shunt (VPS) can range from 32% to 71.4% in these patients.1)3)8)
We describe a CSF diversion strategy and a surgical technique that minimizes hemorrhagic complications associated with VPS in these patients on DAT after placement of flow diverting stents.
OPERATIVE TECHNIQUE
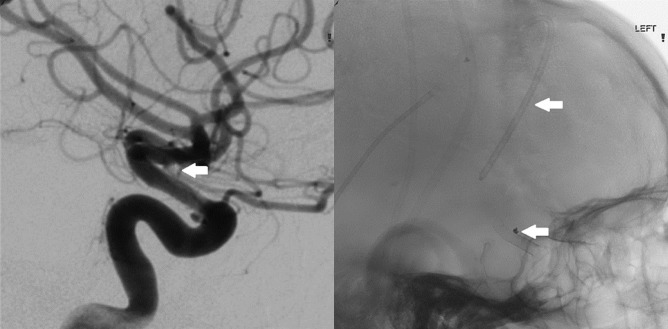
On admission, patients with ruptured cerebral aneurysms are assessed for need of EVD insertion based on their neurological status and radiographic findings in the standard fashion. If an EVD is indicated, it is inserted at bedside in the usual manner using standard anatomical landmark and techniques. After tunneling the ventriculostomy catheter, careful attention is paid to tightly secure the catheter to the scalp. A "purse-string" stitch is first used at the catheter exit site to anchor the catheter; in addition, a catheter loop is formed with 3 additional fixation points on the scalp (Fig. 1) to minimize micro-movement of the EVD catheter intracranially during patient transfer. Patients with ruptured aneurysms treated with flow diverters are maintained on a standard dose of aspirin and clopidogrel. EVDs in these patients are maintained and challenged in the usual fashion.

A photograph demonstrating the catheter fixation technique with a "purse-string" stitch at the exit site to anchor the catheter; in addition, a catheter loop is formed with 3 additional fixation points on the scalp to minimize micro-movement of the external ventricular drain catheter intracranially during patient transfer.
If the clamp trial is successful, the EVD is carefully removed at bedside. We have not experienced any complications with removal of EVDs in patients on DAT. If a patient fails the EVD clamp trial and permanent CSF diversion is indicated, the patient is brought to the operating room without discontinuing DAT. The previous incision at the EVD insertion site is carefully opened with great care to avoid moving the ventriculostomy catheter. The catheter is then cut to an appropriate length proximally close to the burr hole and then connected to a distal VPS system. Any bleeding during the procedure is addressed immediately with electrical cautery.
CASE ILLUSTRATION
Presentation
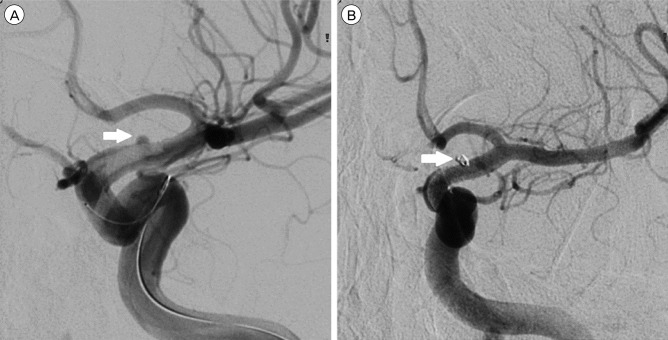
A 32-year-old man with no significant past medical history presented with Hunt-Hess II and modified Fisher Grade 2 (Fig. 2A) subarachnoid hemorrhage (SAH) with radiographic signs of hydrocephalus. On neurological exam he was somnolent but did not have any focal deficit. An EVD was placed at the bedside for CSF diversion (Fig. 2B). Subsequent catheter cerebral angiogram demonstrated a 1.5 mm, wide-necked, left supraclinoid internal carotid artery (ICA) blister aneurysm (Fig. 3A).
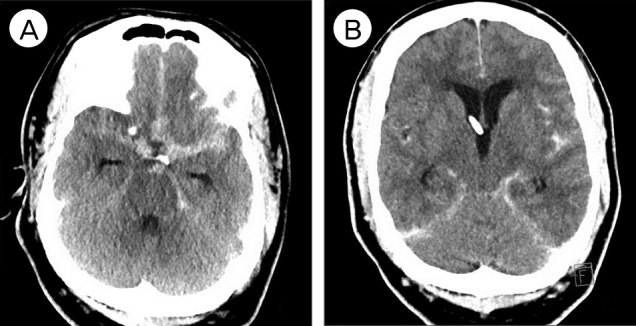
(A) Computed tomography (CT) of brain demonstrating diffuse SAH with enlargement of bilateral temporal horns suggesting the presence of hydrocephalus. (B) CT showing external ventricular drain catheter placement and improvement of ventriculomegaly.
Management
After careful and in-depth discussion regarding both open surgical and endovascular treatment options with the patient and his family, stent-assisted coiling with PED was chosen for treatment of the left ICA blister aneurysm. The patient was brought to the angiography suite and prepped in the usual sterile fashion. Using a Seldinger technique, the right common femoral artery was selectively catheterized using a 6F/10 cm sheath. A 6F guide catheter was used to access the great vessels. A 0.027-inch microcatheter was navigated over a Synchro 14 microwire (Stryker, Kalamazoo, MI, USA) into position across the blister aneurysm. The PED was then loaded into the microcatheter and advanced with the delivery wire. The device was then deployed across the targeted location. Once deployed, the delivery microcatheter was advanced over the delivery microwire to recapture the microwire and re-establish its position across the construct. A microcatheter SL 10 (Stryker, Kalamazoo, MI, USA) and a Synchro wire were used to selectively catheterize and coil the aneurysm. A final angiogram showed Raymond grade I occlusion of the aneurysm (Fig. 3B).
The patient remained neurologically intact after the procedure and was maintained on aspirin and clopidogrel for the newly placed PED. Unfortunately the patient failed the EVD clamp trial at the end of the vasospasm period and required permanent CSF diversion. He was subsequently brought to the operating room for VPS placement. Using the techniques described previously, the proximal ventricular catheter was cut and successfully connected to the distal system without complications. The patient was then discharged home on DAT without complication.
Follow-up
At 6-month follow-up, a repeat catheter cerebral angiogram again demonstrated Raymond I occlusion of the aneurysm (Fig. 4). He remained neurologically intact with no complaints.
DISCUSSION
Surgical procedures in patients on DAT carry increased risk of hemorrhage. Tumialán et al.,8) who reported their experience with EVD and VPS placement in patients on DAT in 2008, found that 5 out of 7 patients (71.4%) developed catheter-related intracranial hemorrhages. Kung et al.,1) who compared complication rates of EVD and VPS placement in patients undergoing endovascular treatment for acutely ruptured cerebral aneurysms, found a significantly higher complication rate in patients with stenting and DAT compared to coiling alone without DAT (32% vs. 14.7%, p = 0.02). Mahaney et al.3) reported similar findings in which 4 of 12 patients (33%) undergoing VPS had a new intracranial hemorrhage associated with catheter placement.
In 2013, Sweeny et al.6) described a catheter fixation and ligation technique similar to ours, which circumvents potential catheter-associated hemorrhages by leaving the proximal EVD catheter in place and connecting it directly to a distal system during VPS. Using this "Cut & Connect" technique, manipulation of the ventricular catheter is minimized and bleeding risk associated with VPS placement in patients on DAT is reduced.
One potential drawback of this approach is potentially higher infection risk. Since the EVD catheter is placed at the bedside instead of in the operating room, the catheter is more likely to be contaminated at time of insertion. This risk can in part be mitigated by use of sterile and meticulous surgical techniques, along with careful daily care of the EVD site. Utilization of an antibiotic impregnated ventricular catheter can further reduce the risk of infection.5) The infection rate of EVDs has been less than 5% at our institution and infection has not been a significant issue. In the rare event that infection occurs, risk of persistent infection will need to be weighed against risk of hemorrhage associated with catheter replacement. "Soft passing" the catheter into the prior EVD tract may be helpful in reducing the risk of bleeding if the ventricular catheter were to be replaced.
CONCLUSION
Flow diverting stents have become a powerful tool in treatment of complex cerebral aneurysms. The "Cut & Connect" technique reduces risk of VPS related hemorrhages in patients on DAT and should be considered in patients with ruptured complex aneurysms undergoing treatment with flow diverters.
Notes
Disclosure: Dr. Roham Moftakhar is a consultant for Covidien; Dr. Demetrius Lopes has financial and research relationships with Covidien, Stryker, and Penumbra; other authors have no conflict of interest to disclose.