Endovascular management of large and giant intracranial aneurysms: Experience from a tertiary care neurosurgery institute in India
Article information
Abstract
Objective
With the development of endovascular technique and devices, large and giant intracranial aneurysms are increasingly being managed by this less invasive method. Here we discuss our experience on managing such aneurysms via endovascular technique.
Methods
Retrospective data on 42 patients with large and giant intracranial aneurysms managed by endovascular techniques between September 2015 to December 2017 at our neurosurgery institute were included in this analysis.
Results
There were a total 42 patients with 9 giant and 33 large aneurysms in this study. Eight aneurysms were treated by parent vessel occlusion, 22 aneurysms with coils and rest 12 aneurysms were treated with stent assisted coiling. Following the procedure, Raymond class I occlusion was accomplished in 31 (73.8%) patients while class Ⅱ in 9 (21.4%) and class Ⅲ in 2 (4.8%) patients. Overall morbidity and mortality were 9.5% and 14.3% respectively and favorable outcome was seen in 80.9% patients. Significant correlation was observed with clinical outcome and initial neurological status.
Conclusions
The study indicates that endovascular intervention is a safe and effective method in managing large and giant intracranial aneurysms with lesser morbidity and mortality.
INTRODUCTION
Large and giant aneurysms are defined as aneurysms between 15 to 25 mm and those having more than 25 mm respectively. They often manifest as a result of catastrophic hemorrhage, mass effect or due to episodes of thromboembolism [9]. Surgical clipping of these aneurysms, though widely performed, is associated with substantial morbidity and mortality because of the size, wide neck or location near or within the cavernous sinus or those having hard atherosclerotic plaque [16,20,22,26]. With the emergence of endovascular therapy the management of large and giant aneurysm has largely been shifted from open surgical approach to the minimally invasive endovascular approach. Endovascular coiling of large and giant aneurysms is a relatively safe and feasible approach and is associated with lesser morbidity and mortality [14,15,24]. With the advancement of modern imaging technology coupled with 3-D reconstruction such aneurysms can be better delineated. Although flow diverters are increasingly being used these days, these devices are still out of reach due to financial constraints in developing countries like India; and coiling is routinely performed at our center which is a tertiary care government institute. Here we report our experience of 42 cases of large and giant aneurysms managed either by coiling or stent-assisted coiling.
MATERIALS AND METHODS
It is a retrospective review of database of patients managed via endovascular technique from September 2015 to December 2017 at our institute. In 282 patients, 308 aneurysms were managed by endovascular technique. Of the total of 282 cases, 42 cases were identified as either large or giant (largest diameter more than 15 mm). Decision regarding whether to treat the cases by coiling or clipping was made by the treating neurosurgeons as both the procedures are performed in our department. However, the decision was predominantly made on the basis of morphology and characteristics of the feeder vessels with posterior circulation aneurysms, small neck, absence of large hematoma requiring evacuation, absence of vasospasm and multiple aneurysms some of the criteria used in favor of coiling. A patient’s demand for the endovascular procedure was even one of the criteria.
All patients at admission were evaluated neurologically using Hunt and Hess (H & H) grade and Glasgow coma scale. Clinical outcomes were evaluated according to modified Rankin Scale (mRS) score measured at 3rd month after the initial procedure. Achievement of mRS score of 0-2 was designated as favorable outcome while score of 3-6 was defined as unfavorable outcome.
Computed tomographic angiography and digital subtraction angiography (DSA) of the brain was performed in all patients at our department. On pre-operative DSA, routine note was made regarding the neck, width, height, location, morphology of the aneurysms and the cross flow.
The endovascular treatment of all aneurysms were performed with a standard technique under general anesthesia using 6-7 diagnostic catheter Cook (Cook Inc., Bloomington, IN, USA) and Cordis (Miami Lakes, FL, USA) and 7-F sheath, micro-guide wires of size 10 and 14 Transcend (Boston Scientific, Natick, MA, USA), Agility (Cordis, Miami Lakes, FL, USA) and Mirage (EV3, Plymouth, MN, USA) along with micro-catheter, Prowlers series and Prowler plus (Johnson & Johnson, Miami Lakes, FL, USA) as described by us in our previously published article [23]. After creating basket with 3 D coils, sufficient packing of the aneurysm was performed until no contrast was apparent in more than one place inside the sac. We used electric (Boston Scientific, Fremont, CA, USA), hydraulic (Microvention) as well as mechanical detachment systems. Stents used in the procedures were either of Solitaire (ev3), Neuroform (Boston Scientific, Natick, MA, USA) and Enterprise (Codman & Shurtleff, Inc., Raynham, MA, USA). Angiographic outcome was evaluated using Raymond class as complete obliteration (class I), residual neck (class II) and residual aneurysm (class III).
The peri-operative antiplatelet therapy in ruptured aneurysms consisted pretreatment of 150 mg acetylsalicylic acid and 450 mg clopidogrel given 3-5 days before surgery as well as an hour after coil embolization via nasogastric tube and continued for a month when stentassisted coiling (SAC) was employed and for 6 months in parent vessel occlusion (PVO). We routinely used bolus of 5000 IU heparin immediately after insertion of femoral catheter intra-arterially followed by infusion of 1000 IU of heparin per 500 mL normal saline (0.9%) during the entire procedure. Continuous intravenous infusion of nimodipine at 5 mg/h was also administered throughout the procedure and continued post-procedure to prevent vasospasm. Large and giant aneurysms were defined as those with diameter greater than 15 mm and 25 mm respectively as measured by DSA. All patients were analyzed regarding the size and type of aneurysm.
At our institute, we perform balloon test occlusion (BTO) whenever permanent PVO is required and the patient should tolerate the procedure before he is deemed fit for PVO. We performed BTO in awake, heparinized patients under local anesthesia and assessed the neurological status of the patient post-procedure and noted the angiographic status of the vessels. A delay of >4s of venous drainage between the territories of the artery that has been injected and the occluded hemisphere was considered as cutoff for ineligibility for PVO, as described in another study [27].
Statistical analysis
Comparisons among different groups were analyzed by the use of paired t tests and statistical significance was defined as a probability value 0.05. Statistical analysis was done by SPSS (version 19.0, IBM Corp., Armonk, NY, USA).
RESULTS
Patient characteristics
There were total 42 patients with 42 large or giant aneurysm. Of them, 15 (35.7%) were male and 27 (64.3%) were female with a mean age of 47.8 years. There were 9 patients with giant aneurysms and 33 patients with large aneurysms. Six patients were admitted with symptoms associated with unruptured aneurysm and 36 patients were admitted with symptoms of subarachnoid hemorrhage. According to H & H grading 6 patients were in Grade 0, 11 in Grade I, 8 in Grade Ⅱ, 9 in Grade Ⅲ and 8 in Grade Ⅳ (Table 1). Endovascular treatment with or without SAC or PVO was performed within 72 hours in all of 36 patients with ruptured aneurysms. Of the 6 patients having unruptured aneurysms, 2 presented with symptoms of visual deficits and 4 presented with symptoms of compression with 3rd nerve palsy. Of the 36 patients with ruptured aneurysms, 5 (13.9%) patients had features of neurological deficits due to mass effect of the aneurysms and 3 (8.3%) had features of ischemia.
There was a total of 35 (83%) aneurysms, either giant or large that were located in anterior circulation and 7 (27%) aneurysms that were located in posterior circulation. In the anterior circulation, internal carotid artery (ICA) supraclinoid aneurysms were present in 20 (47.62%) patients whereas basilar top aneurysms topped the list in posterior circulation found in 5 (11.9%) patients (Table 2). The size of the aneurysms ranged from 15 to 28 mm. There were 35 (83.3%) saccular aneurysms and 7 (16.7%) fusiform aneurysms. There was one patient with a multilobulated aneurysm and one with bilobed aneurysm.
Endovascular procedure
All the 42 patients underwent endovascular management with the aim of alleviating symptoms and controlling further aneurysmal growth and a possible future bleed and mass effect due to the aneurysm. Eight aneurysms were treated by PVO, 22 aneurysms with coils and rest 12 aneurysms were treated with SAC. Immediately after the procedure, Raymond class I occlusion was accomplished in 31 (73.8%) patients while class Ⅱ in 9 (21.4%) and class Ⅲ in 2 (4.8%) patients. After recoiling was attempted in 2 of the class Ⅲ giant aneurysm patients, class Ⅱ result was obtained in one of them. Categorically, class I occlusion was achieved in 8 out of 8 (100%) of PVO cases, 9 out of 12 (75%) SAC cases and 14 out of 22 (63.6%) of coiling alone cases (Table 3).
No intra-procedural mortality, iatrogenic dissection or aneurysmal rupture was seen in this study; however, stent-associated vasospasm was seen in 2 patients and coil protrusion was seen in 3 patients.
Clinical and angiographic outcome and follow-up
Every patient underwent angiographic evaluation after the procedure to assess the aneurysm obliteration and patency of the parent vessels. Follow-up angiographic studies were obtained for 1-34 months (mean, 10.6 months). The mRS score at 3rd month post the initial procedure ranged between 0-2 in 32 (80.9%) and 3-6 in 10 (19.1%) patients respectively. Overall morbidity and mortality were 4 (9.5%) and 6 (14.3%) respectively and favorable outcome was seen in 32 (80.9%) patients. In all the 6 unruptured aneurysm cases, there was good clinical and angiographic outcome. Of the 6 patients who died in the hospital, 4 had massive brain edema with increased intracranial pressure due to initial subarachnoid hemorrhage and not because of procedure related complications; on admission they had a poor H & H grade and were taken up for coiling due to large aneurysm size with massive subarachnoid hemorrhage. Delayed thrombotic occlusion occurred in two patients for which they underwent decompressive hemicraniectomy. Both the patients however died later.
In 3 patients there were partially thrombosed aneurysms and both were in anterior circulation. In 2 of them, PVO was performed and in one it was coiled. The latter patient developed infarction probably due to thromboembolism and decompressive hemicraniectomy was performed later.
All the 36 surviving patients were clinically followed for a mean of 12.7 months (range, 6-34 months) after the procedure. During this follow-up period, two patients had major recanalization between 10 and 16 months and both were successfully re-treated by coiling alone. Clinical outcome of the patients was related to neurological status at admission with mRS 6 seen only with Hunt and Hess grade 5 or 6 (p=0.02) while outcome of the procedure was not significantly related to the size of the aneurysm sac (p>0.05). Two illustrative cases are shown in Fig. 1 and 2.
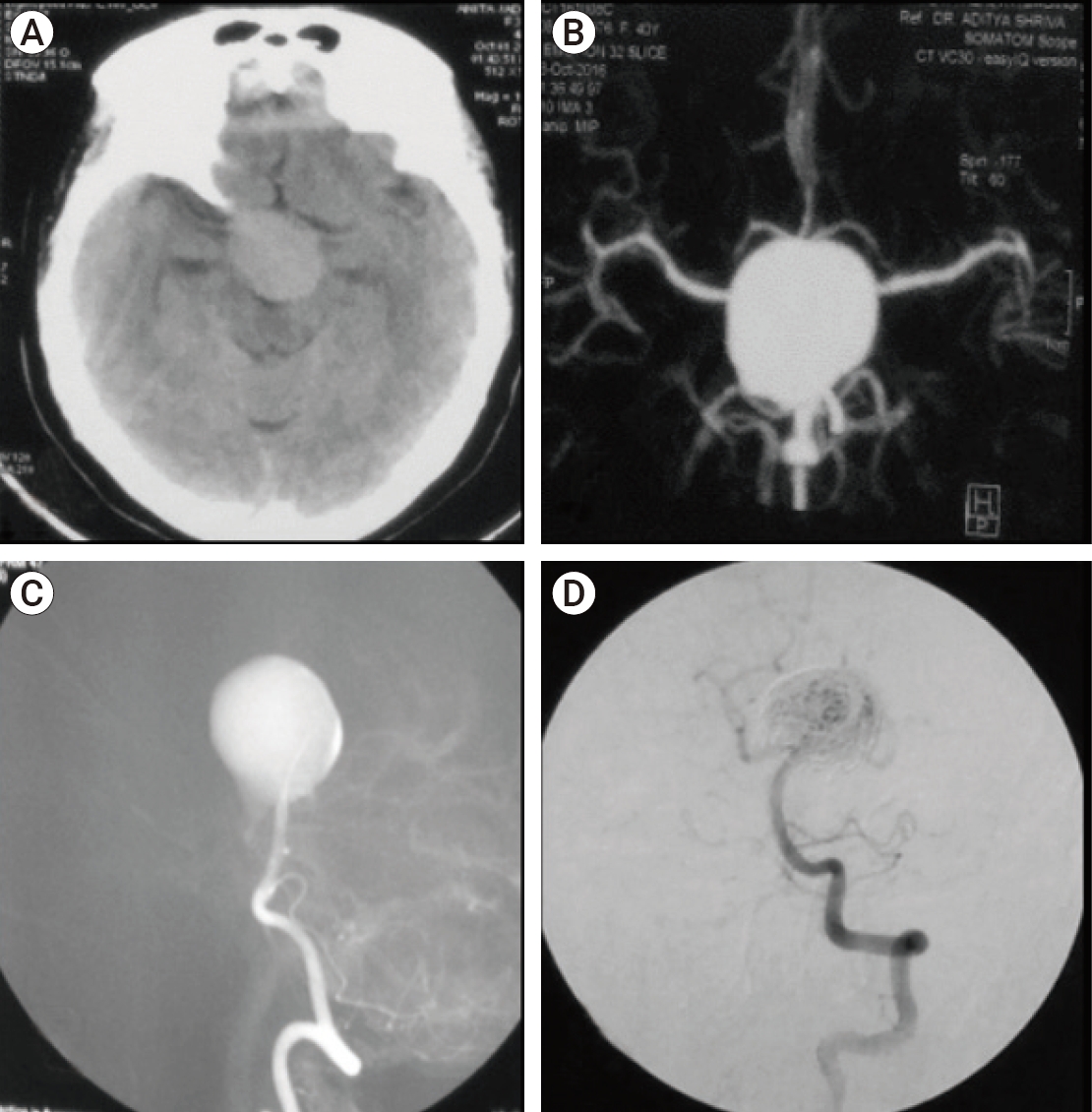
(A) Non-contrast computed tomography brain showing a slightly hyperdense area anterior to the midbrain. (B) CT Angiography brain showing a giant saccular aneurysm but the site of origin could not be established. (C) DSA showing a basilar top aneurysm filling from the left vertebral artery. (D) Post coiling DSA showing decreased filling. CT, computed tomography; DSA, digital subtraction angiography.
DISCUSSION
Large and giant intracranial aneurysms pose a major treatment challenge for the cerebrovascular neurosurgeons. These aneurysms in the internal carotid segment have a high blood flow velocity and are difficult to treat. In the posterior circulation, basilar top aneurysms have a wide neck and coiling of these aneurysms may become technically difficult sometimes requiring stents for support. Patients who present with ischemic symptoms secondary to hemodynamic insufficiency due to aneurysm in anterior circulation treated by permanent ICA occlusion can be improved by external carotid-internal carotid bypass done before the occlusion procedure as found in one study [2] and this seems relevant as we lost 2 patients due to delayed thrombotic occlusion. These two patients had shown good cross flow on preoperative DSA and after complete occlusion of the aneurysm the cross flow was also present. For some failed or uncoilable/unclippable large or giant ICA aneurysms, this bypass technique remains a feasible option as suggested by some studies although sometimes the results of this multidisciplinary approach remain relatively inferior compared to that of smaller aneurysms [8,11,18,28].
In view of the recent development of new endovascular devices these large or giant ICA aneurysms can be treated with low morbidity and mortality. SAC is emerging as an alternate method for PVO as the latter is not tolerated in a vast number of cases [7,24]. This technique can however lead to possible damage in the parent artery in some cases. Results of SAC of unruptured larger or giant intracranial aneurysms is encouraging as well as safe and averts the aneurysm from a possible rupture [24].
Framing a treatment strategy for large and giant aneurysms is difficult because of lack of large clinical trials and both open microsurgical and endovascular approaches exist. Microsurgical options are effective in immediate dome occlusion but are associated with significant morbidity [13] while endovascular treatment with conventional coils or with flow diversion has inherent risks of recurrence or aneurysmal regrowth [3]. Dengler et al. [6] conducted a meta-analysis on outcome of both surgical and endovascular approaches in giant aneurysms and found that overall good outcome is above 80% in both microsurgical and endovascular treatments while with increasing patient age, the chances of favorable outcome tends to fall. Another study found that although microsurgical clipping provides better results in terms of re-bleeding, and re-treatments, endovascular approaches are in terms of post-operative complications and favorable outcomes [1].
Coiling, however cannot abate the mass effect due to compression of some large aneurysms [7]. In our study cohort, we performed SAC successfully with under packing of these aneurysms and the third nerve palsy due to this mass effect improved until near complete improvement after three months from the endovascular treatment.
Balloon and SAC techniques have been one of the milestones in the endovascular treatment of complex intracranial aneurysms but at present flow-diversion devices represent the latest revolution in treatment of endovascular aneurysms and the treatment is changing from aneurysm embolization to parent vessel reconstruction specially in fusiform aneurysms [17]. The early results reported in wide-necked large or giant proximal intracranial aneurysms and fusiform aneurysms treated using this device have been extremely encouraging [5,7,10,17,19,25,29]. However, flow-diversion devices have their own disadvantages like occurrence of stroke during the procedure or even rupture; hence this method is not invariably the safest or most successful method. Uninterrupted blood flow through the perforators following the procedure also remains unproven [17,29]. One of the most relevant international study assessed neurologic complication rates following Pipeline Embolization Device and found that procedure-related morbidity and mortality are higher in the treatment of giant aneurysms [12]. Peschillo et al. [21] treated 44 patients of large or giant ICA aneurysms with flow diversion either alone or with combination with coils and found that 88.6% of the patients had a favorable outcome at one-year post-procedure. Another study4) reported a procedural-related mortality of 4% with these devices. The flow diversion devices are still being improved upon and the perfect device to treat aneurysm is yet to come.
In partially thrombosed aneurysms the PVO was a better procedure as there was no morbidity following it. In one case where the partially thrombosed aneurysm was occluded by coils, thromboembolism occurred which would have been due to the dislodgment of a part of thrombus during placement of microcatheter or when the coils were deployed.
CONCLUSIONS
Coiling or SAC of large and giant aneurysms is associated with reasonably low morbidity and mortality in good H & H grade patients. The flow diversion devices are a promising method to treat such aneurysms but the drawback of them are that they are costly and out of reach to the common man. Better yet inexpensive endovascular devices are needed to obtain more secure occlusion.
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.