A Ruptured lenticulostriate artery aneurysm in moyamoya disease treated with Onyx embolization
Article information
Abstract
Lenticulostriate artery (LSA) aneurysms are uncommon. Here, we report one case of ruptured LSA aneurysm which is related to Moyamoya disease (MMD). Surgical treatment of this aneurysm is challenging because of its deep location and complex neural structures around the LSA. We report one case treated with endovascular Onyx embolization, successfully and review LSA aneurysm associated with MMD.
INTRODUCTION
Lenticulostriate artery (LSA) aneurysms are uncommon. So, deep intracranial hemorrhage due to ruptured LSA aneurysms is also rare. According to a systemic review article published by David E. H-G et al. in 2021, 112 cases were reported in 71 previously related articles and 78% of 112 cases were presented rupturing [1]. The optimal treatment of this entity remains to be elucidated; however, if we can safely prevent repeated re-bleeding, most patients can achieve good neurological recovery or maintain a stable functional status. So, we can consider endovascular or surgical treatment beside closed conservation [7]. Here, we report one case of ruptured LSA aneurysm which is related to Moyamoya disease (MMD). Surgical treatment of this aneurysm is challenging because of its deep location and complex neural structures around the LSA. There are few LSA aneurysm cases treated with Onyx embolization. We report one case treated with Onyx embolization, successfully and review LSA aneurysm associated with MMD.
CASE REPORT
A 42-year-old man sought treatment in the emergency department for the acute onset of headache and nausea. He had no history of headache and chronic underlying diseases such as hypertension or diabetes etc. He had also no specific medication history. On neurologic examination, the patient was intact, neurologically.
Computed tomography (CT) of the head at admission revealed an intraventricular hemorrhage (IVH) extended from a focal hemorrhage in the body of the corpus callosum (Fig. 1). He was young and had no risk factor for intracerebral hemorrhage (e.g., hypertension, diabetes). Therefore, enhanced magnetic resonance images (MRI) was performed. We found enhanced vascular spot point which can be origin of IVH in lateral wall of the right frontal horn (white arrow in Fig. 2). Trans-femoral cerebral angiography (TFCA) was performed. A left internal carotid injection demonstrated a total occlusion of the distal internal carotid artery with numerous basal collateral vessels. A right internal carotid injection revealed a total occlusion of the proximal A1 segment, and the distal anterior cerebral artery territory was supplied with ethmoidal collateral vessels. All these findings were consistent with MMD (Fig. 3). A ruptured saccular aneurysm which causes IVH was found in the LSA arising from proximal one third of right middle cerebral artery (MCA) (white arrow head in Fig. 4). Initially, conservative treatment was selected based on his neurological condition, with expectation of spontaneous regression. A repeat TFCA performed on post-hemorrhage day 18 demonstrated persistent filling of the aneurysm, and the patient’s clinical status was unchanged.
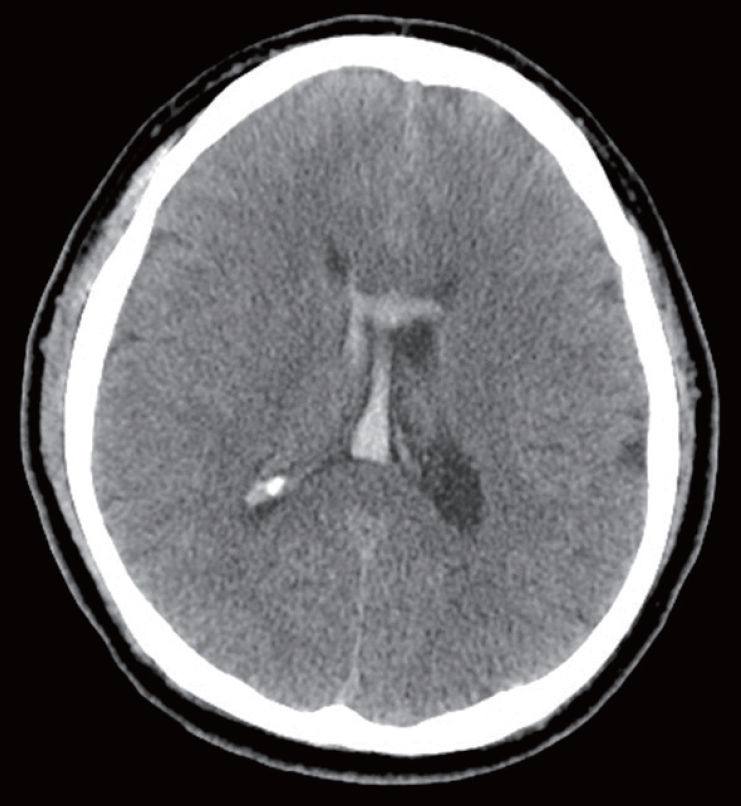
Axial view of brain computed tomography (CT) image is showing acute intraventricular hemorrhage (IVH) with focal hemorrhage in the body of the corpus callosum.
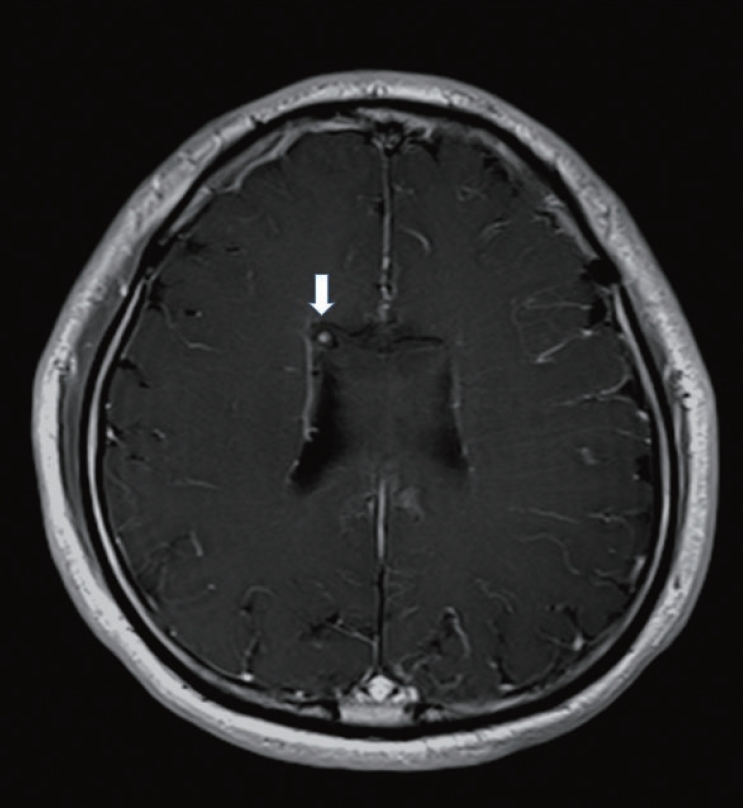
Axial view of enhanced T1-weight magnetic resonance image (MRI) is showing abnormal vascular spot point which can be origin of intraventricular hemorrhage in lateral wall of the right frontal horn (white arrow).
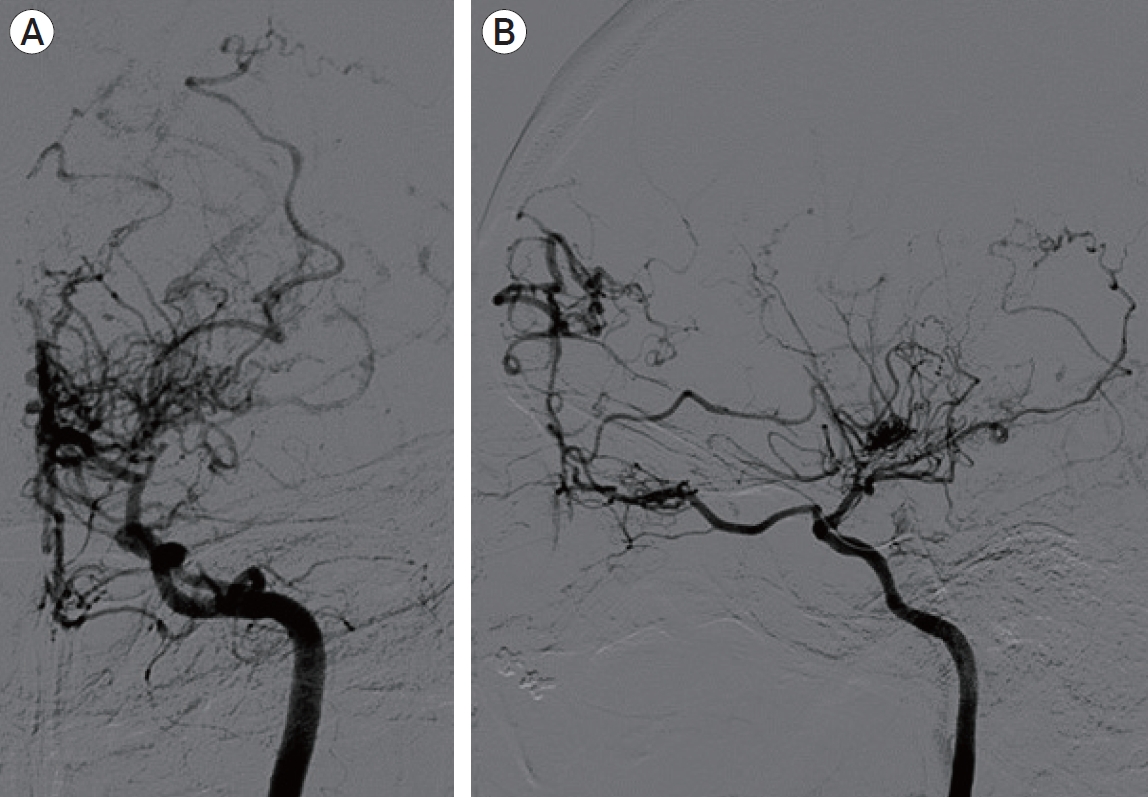
Left internal carotid artery (ICA) digital subtraction angiography (A) frontal and (B) lateral projections are confirming a total occlusion of distal ICA segment with numerous basal collaterals and the distal ACA territory was supplied with ethmoidal collateral vessels which is compatible with moyamoya disease. ACA; anterior cerebral artery.

Preoperative right internal carotid artery (ICA) digital subtraction angiography (A) frontal and (B) trans-orbital oblique projections are showing a ruptured saccular aneurysm (white arrow head) was originated in the lenticulostriate artery (LSA) arising from proximal one third of right middle cerebral artery (MCA). The LSA was too tortuous and acute angle (white arrow) made by MCA to advance the guidewire. Unlike the left ICA, which showed typical MMD findings in Fig. 3, the right ICA showed almost normal distal patency. So, we diagnosed this case as probable MMD.
In consideration of the location of this deep-seated aneurysm and fragile MMD vessels, we decided endovascular treatment. An attempt was made to select the LSA; however, the LSA showed too tortuous and acute angle (white arrow in Fig. 4) made by MCA to advance the guidewire. Therefore, we devised the “Balloon bumping guidewire advancing technique” and decided to perform the procedure (Fig. 5). As we know, this technique may be the 1st description which our team devised in 2017. This technique has two key steps. The first step is micro-wire selection using balloon bumping (we can make artificial wall which supports micro-wire advancing. The second step is jailing micro-catheter using balloon to prevent micro-catheter kick-back. We positioned the Gateway PTA Balloon Catheter (Boston Scientific, Fremont, California, USA) just distal to the ostium of the targeted LSA. The Mirage-10 micro-wire (Ev3, Irvine, California, USA) was bumped against the balloon, flexed, and advanced along the LSA, and the Marathon 10 micro-catheter (Ev3, Irvine, California, USA) was positioned just proximal to the LSA aneurysm. With Onyx injection, the distal LSA aneurysm was embolized. There was no evidence of embolic material reflux. Post-embolization angiogram showed no aneurysmal filling. Patent collateral vessels of the LSA were also confirmed (Fig. 6). After the intervention, the patient’s neurologic status was remained stable and unchanged, and the patient was discharged on postoperative day 3. At 3-month clinical follow-up, the patient was neurologically stable and at 3-year MRI follow-up, the complete occlusion of aneurysm was maintained.
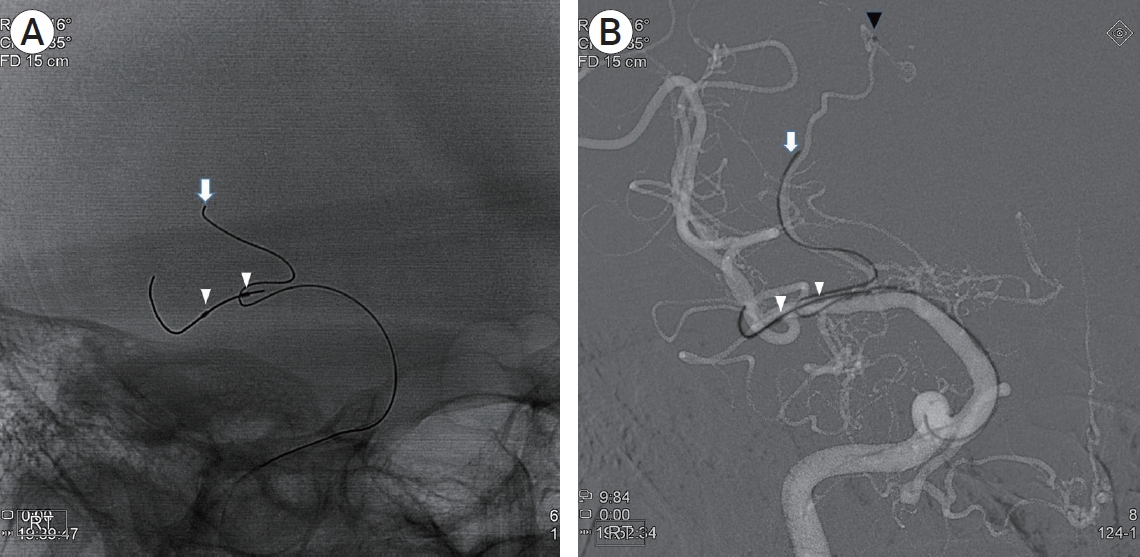
“Balloon bumping guidewire advancing technique”: We positioned the Gateway PTA Balloon Catheter (white arrow heads: proximal & distal markers of balloon) in the middle cerebral artery (MCA) just distal to the ostium of the targeted lenticulostriate artery (LSA). The Mirage-10 micro-wire (white arrow) was bumped against the balloon and advanced along the LSA (A: plane image) and the Marathon 10 micro-catheter (black arrow head: marker of tip) was positioned just proximal to the LSA aneurysm (B: roadmap image). We fixed the micro-catheter with balloon, firstly and removed the micro-wire, gently. There was no change in position of micro-catheter tip (C: plane image). With Onyx (black arrow) injection, the distal LSA aneurysm was embolized (D: reverse-roadmap image).
DISCUSSION
A hemorrhagic stroke in normotensive patients younger than 50 years is caused by a structural abnormality in up to 83% of cases [2]. A cerebral angiography was therefore warranted in the described case and did reveal a LSA aneurysm in the setting of MMD.
Incidences of intracranial aneurysms in MMD have been estimated to be 3–14% in adults [6]. According to Kawaguchi et al., aneurysms associated with MMD can be classified into two types, which include aneurysm of the major artery aneurysm (60%) and blood flow secondary to the arterial stenosis (40%; choroidal, moyamoya vessels, meningeal vessels) [3]. The aneurysms on the major artery aneurysm usually present with subarachnoid hemorrhage, while aneurysms on the peripheral arteries with intracranial or intraventricular hemorrhage. Aneurysms of the LSA are rare. The etiology of LSA aneurysms remains unknown. However, they can be associated with specific vascular abnormalities such as arteriovenous malformations and MMD or systemic vasculitis including systemic lupus erythematosus [1]. LSA aneurysms in patients with MMD are most commonly distal, thereby manifesting as a hemorrhage in the basal ganglia area, but in this described case intraventricular hemorrhage was manifested.
Hemodynamic stress was involved in the development of such aneurysms in MMD. Worsening occlusion of the ICA compromises the flow dynamics in unobstructed arteries, with compensatory dilation and blood flow in the MMD vessels. This increased flow often results in elevated blood pressure and the formation of an aneurysm. Rupture can also be occurred due to persistent hemodynamic stress on dilated, fragile MMD vessels [4]. Many treatment options are available such as observation, surgery, or endovascular therapy.
Since the fragile MMD vessels, interruption of anastomotic channels, poor tolerance to retraction and ischemia, and poor reserve capacity of hemodynamics could be the obstacles for the clipping procedure. Endovascular treatment is less invasive and has shown good results for major artery aneurysms associated with MMD in adults. But micro-catheter access to LSA is quite difficult, endovascular treatment remains challenging.
In our case, we used Onyx material for ruptured LSA aneurysm. As mentioned in several previous case reports, Onyx allows longer, slower, and more controlled injections with its non-adhesive nature [5].
We could effectively use Onyx because we closely positioned the micro-catheter tip to the aneurysm with “Balloon bumping guidewire advancing technique”. If we failed to select the acute angled parent LSA with the micro-catheter, we could not perform endovascular treatment, successfully. NBCA could also be option for embolic material. Theoretically, it can penetrate more distally along the vessel, but it is easy to make risky reflux to MCA due to so small diameter and caliber of the parent LSA. Coil embolization was not an option. Because of the so small caliber of the parent LSA, we could not perform the direct selection of aneurysmal sac, moreover, MMD vessels are too fragile to fill coils.
There was no procedure related infarction in follow up MR. Theoretically, occlusion of only the aneurysm sac is an ideal goal, but this case is a ruptured fusiform aneurysm that has a fairly saccular shape, but also has retrograde filling. Because we needed the lesion segment trapping, we planned lesion fenestration using liquid embolic material. In order to prevent infarction as much as possible, short segment trapping should be performed, so Onyx is used rather than glue, which is easy to handle retrograde reflux and has good visual expression. I think that glue can be another option, depending on the situation.
CONCLUSIONS
Treatment of LSA aneurysm with either microsurgical or endovascular surgery is challenging due to its deep location and fragility of MMD vessels. Onyx embolization can be an effective treatment of aneurysms associated with MMD. We could effectively use Onyx with optimal position of micro-catheter tip through “Balloon bumping guidewire advancing technique” which we devised.
Notes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.

