 |
 |
| J Cerebrovasc Endovasc Neurosurg > Epub ahead of print |
Abstract
Intracranial aneurysm is common in stroke and, once rupturing, will cause disaster to patients. Nowadays, endovascular treatment has become a routine to reduce the risk of intracranial aneurysms rupture. Successive endovascular methods, like balloon-assisted coiling, stent-assisted coiling, and flow diversion, have become new choices for doctors. More and more doctors have been entering this field. Understanding the current general situation is crucial for more medical workers to learn the endovascular treatment of intracranial aneurysms. In the past, many devices and ideas about the treatment of intracranial aneurysms appeared. Although developing unceasingly, endovascular treatment still has some deficiencies to overcome. The advantages and drawbacks of current endovascular methods are discussed.
Intracranial aneurysm is a crucial disease that tremendously burdens families and health systems. Despite geographical locations or ethnicity, the non-comorbidity overall prevalence of unruptured intracranial aneurysms (UIAs) is approximatively 3-5% in the population [69]. UIAs are more prevalent in women than in men and there are no differences in age, expect for the under 30 years patients [69]. Once intracranial aneurysms rupture, subarachnoid hemorrhage often occurs in the brain. According to a recent prospective observational study [56], based on current treatment guidelines, patients with aneurysmal subarachnoid hemorrhage have a 5-year mortality of 29%, and just 64% of these patients were alive without disabilities at a 5-years follow-up. Nevertheless, with the development of medical techniques, the case fatality of aneurysmal subarachnoid hemorrhage has been declining. According to a meta-analysis of 33 articles, case fatality has decreased by around 23% between 1972 to 2003 [45].
There are two types of treatment: neurosurgical treatment and endovascular treatment (EVT) (Fig. 1). Surgical clipping was once considered as the gold standard; however, with the appearance and prevalence of alternative endovascular treatment, the status of surgical clipping is challenged. Nevertheless, surgical clipping is still a safe and effective method to treat aneurysms. Endovascular treatment also has many disadvantages, such as recanalization, bleeding during the operation. Especially in the treatment of complex intracranial aneurysms, endovascular therapy has many limitations. In postoperative patients with UIAs, its mortality is around 1-3%, and its rate of unfavorable outcomes (including death) is around 7% [30] and some claim that in low-risk cases, microsurgical treatment is a preferential choice [29].
In 1990, the first endovascular device appeared in clinical practices [20] and it is gradually becoming prevalent compared with neurosurgical treatment [7,34]. A meta-analysis [44], including 5,044 patients with UIAs from 71 studies, showed that EVT-associated mortality is around 2%, and the rate of unfavorable outcomes (including death) is around 4.8%.
Since the introduction of this new method in clinical use, many studies compared neurosurgical and endovascular treatments. In the field of aneurysmsŌĆÖ rupture, the International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling started as early as 1994 [38,40]. The ISAT randomly assigned 2143 patients with ruptured intracranial aneurysms to neurosurgical clipping (n=1070) or endovascular coiling (n=1073). Two months after treatments, 26.1% of patients who were allocated to EVT and 36.9% of patients who were allocated to neurosurgery were known to be dead or dependent (relative risk=0.71). One year after treatments, 23.5% of patients who were allocated to EVT and 30.9% of patients who were allocated to neurosurgery were known to be dead or dependent (relative risk=0.76). Among the patients who were allocated to EVT or neurosurgery, case fatality rates in the first years were around 8% and 10%, respectively. Furthermore, it seems that there were more likely deaths allocated to neurosurgery than EVT within the first seven years. Both risks of late rebleeding are low, though the risk is more common after EVT. In 2015, a follow-up article [39] of the ISAT concluded that the ten yearsŌĆÖ possibility of disability-free survival was significantly higher in the EVT group compared with that in the neurosurgical group. In 2013, a meta-analysis on ruptured intracranial aneurysms [32] that included 11,568 patients from 27 studies, concluded that EVT generates a better clinical outcome than neurosurgical treatment, and that EVT leads to a higher risk of rebleeding. In 2018, a systematic review on aneurysmal subarachnoid hemorrhage [33] that included 2,458 patients from 4 randomized controlled trials, concluded that if the aneurysm is suitable for both EVT and neurosurgical clipping, EVT is associated with a better outcome. In the field of UIAs, some studies were carried out simultaneously and a recent meta-analysis [1] that included 106,433 patients from 144 studies about UIAs, concluded that among patients allocated to EVT or neurosurgery, the risks of procedural clinical complications (including death) were 4.96% and 8.34%, respectively. However, the case-fatality rates of both were similar (0.3% and 0.1%, respectively).
It seems that EVT is the best choice for patients with UIAs or ruptured aneurysms; however, it is still a complicated procedure for clinical strategy, especially for patients with UIAs who face the decision of whether to choose conservative management or interventional treatment. Some studies suggested that most UIAs do not rupture [75]. Moreover, a study [2] sent questionnaires to patients with UIAs who received preventive treatments (including EVT and neurosurgical treatment) and found that some patients suffered a reduction in life satisfaction during the post-treatment recovery period. Approximatively 19% of the patients did not recover to preintervention functioning, and approximatively 22% of the patients who were employed before aneurysm treatments cannot work like before. However, risk factors for aneurysm rupture should be considered, especially independent risk factors, including age, hypertension, history of subarachnoid hemorrhage, aneurysm size and location, and geographical region [19]. Some risk factors for aneurysm rupture, such as smoking, a family history of intracranial aneurysms, genetic factors, aneurysm shape or morphology, and the direction of blood flow into the aneurysm, are also important [14]. Before EVT, factors associated with complications from EVT, female, diabetes, hyperlipidemia, cardiac comorbidity, wide aneurysm neck, posterior circulation aneurysm, stent-assisted coiling, and stenting, should be considered [1]. Meanwhile, patientsŌĆÖ thoughts and anxiety are worthy of consideration, and therefore, it is important to individualize treatments.
Traditional EVT is a procedure which involves putting coils into intracranial aneurysms. To achieve this procedure, operators use a catheter with a small diameter to deliver coils. When coils arrive at the aneurysms, they will be released and packed. In the first reported endovascular treatment, operators used electrolytically detachable coils, which are made of platinum and depend on the electrolytic detachment method [20]. Then with the development of EVT, more advanced materials, designs, and detachment methods appeared.
One of the most prevalent materials is platinum-based material. This marvel material performs well, overwhelming the use of other metal materials. Due to their chemical stability, platinum-based materials rarely corrode in physiological environments or cause allergic reactions. They can be made into 25 m size material, while also maintaining a similar mechanical strength. Furthermore, platinum can be clearly seen in X-ray images during an operation because of its radiopacity [78]. Unlike magnetic metals, platinum can be carried into magnetic resonance imaging (MRI) devices, which brings convenience to patients.
Regarding the structure, due to the fragility of the aneurysm wall, coils should be soft enough and decently increase the Intrasaccular pressure. Meanwhile, the structure should keep stiff facing the blood flow to prevent recanalization. Many coils are designed to improve embolism outcomes by promoting blood coagulation or increasing packing densities [78].
Electrolytic detachment has some drawbacks. For example, time spending is uncertain, and sometimes detachment needs several attempts to succeed. Moreover, gas generated from electrolysis may cause clot formation [78]; however, the appearance of hydraulic and mechanical detachments has solved these annoying problems.
The primary coil system, also known as Guglielmi detachable coil (GDC), is a typical coil. A study [66] that followed 141 aneurysms in 130 patients who were treated with GDC between January 1995 and August 1999 showed that occlusion rates after six months or longer were 100% for 61%, more than 95% for 22%, and less than 95% for 17%. Just one recurrence occurred on the 6-month follow-up angiogram. However, another study [52] that followed 501 aneurysms in 466 patients who were treated with GDC between August 1992 to May 2002 showed that the rate of complete occlusion after 12 months is 38.3%, and the rate of recurrences is 33.6%. In 2013, a meta-analysis [55] from 104 studies that included 22,134 aneurysms treated with bare coils, concluded that the overall unfavorable angiographic outcome rate was 17.8% (the unfavorable angiographic outcome is defined as any degree of recurrence).
Various materials, such as polyglycolic acid (PGA), polylactic-co-glycolic acid (PLGA), nylon, or expandable hydrogel, have been applied to improve occlusion rates and avoid recurrence. These newer coils are called bioactive coils.
Nevertheless, the appearance of these named bioactive coils caused huge controversy due to their availability on the market without valid clinical trials [12,53]. A study that performed a systematic review of the literature from 2002 to 2007 reported the following statement regarding the products: ŌĆ£illustrates the failure of the industry, the regulatory authorities, and the neuro-interventional community combined to provide a reliable and prudent approach to the introduction of new devicesŌĆØ [74].
In 2008 and 2011, two reports [72,73] on a hydrogel coil trial indicated that hydrogel coils are safe and lower major recurrence, but whether they improve long-term clinical outcomes was not clear. In 2008, a trial [68] about Nexus coils (coils with PGLA microfilament threads) showed that PGLA has no effect on reducing recurrence. In 2013, a meta-analysis [54] from 82 studies between 1999 and 2011, claimed that coil type does not significantly affect angiographic follow-up outcomes. Besides, bioactive coils may induce headache and fever due to their inflammatory effects [63].
However, new bioactive coils have been evolving. In 2016, a meta-analysis [8] that included 2168 patients of 5 randomized clinical trials between 2011 and 2014, showed that bioactive coils have a high rate of a complete aneurysm occlusion and a reduced the rate of residual neck aneurysms in the mid-term when compared with bare coiling. Nevertheless, a recent 5-year follow-up randomized trial that included 580 patients compared the effectiveness of bioactive coils (Matrix2) to bare coils and showed that there is no significant difference between bioactive coils and bare coils [36].
While coil is prevalent among filling materials, it also has disadvantages. Volumetric ratio (coil/aneurysmal volume) is a crucial index that may determine the possibility of recanalization [64,67]. Although it is entirely possible to fill the aneurysm, the volumetric ratios of coils are less than 37% [49]. However, with the help of balloon-assisted or stent-assisted coiling, the risk of coil protrusion dramatically decreased. Nevertheless, it makes the procedure more time-consuming.
In 2006, an experimental endovascular treatment used a liquid material called thermoreversible gelation polymer and succeeded [62]. Then, other hydrogel embolic materials proved their effectiveness in vitro [3,4,50,51]. No clinical trial has assessed the practicability of hydrogel materials, though hydrogel material is considered a promising material [27].
In 2015, a study assessed two new devices, called the coil-in-shell and the gel-in-shell, in porcine sidewall aneurysms [37]. The devices comprise coils or hydrogel surrounded by a shell composed of hyaluronic acid and polyurethane copolymer. They performed well in minimizing aneurysm recurrence. This study suggested that coil-in-shell or gel-in-shell depends on the stimulation of tissue coverage at the neck rather than a complete initial occlusion which can eventually facilitate aneurysm occlusion and neointimal healing.
There are some limitations in coiling without stent assistance, such as the recanalization high risk, the slow neointimal healing, and the crucial drawback that cannot be performed in complex aneurysms, especially in wide-necked aneurysms due to the high risk of coil protrusion.
The initial use of stent was aimed at preventing coil out from aneurysms. In early 2000, a technical note [16] showed the application of stents in the treatment of intracranial aneurysms. Then, some stents for intracranial aneurysms were introduced into clinical practice.
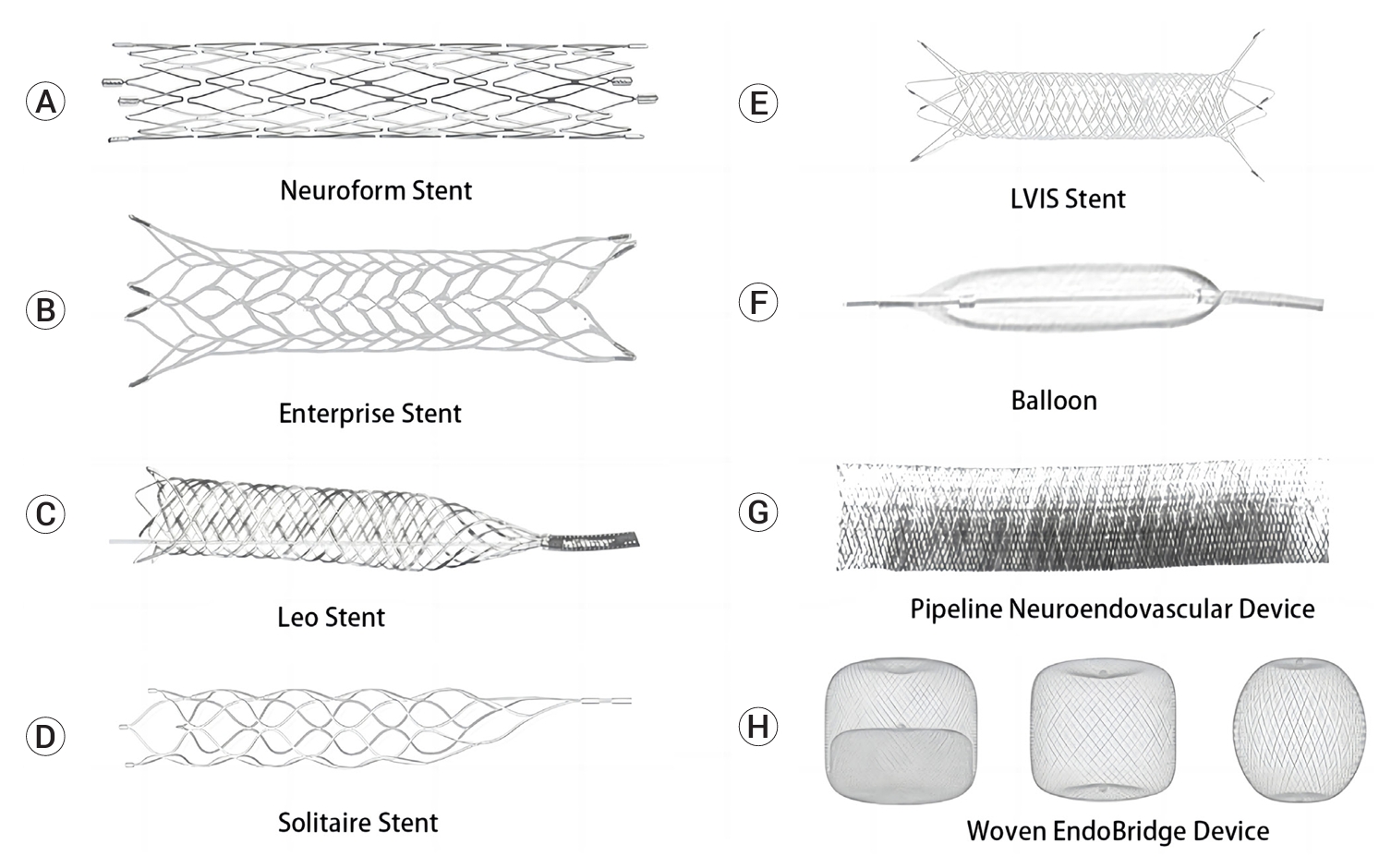
The common materials of the stent for aneurysms are nickel-titanium alloys (nitinol), cobalt-based alloys, and stainless-steel alloys. Generally, self-expandable stents use nickel-titanium alloys, while balloon-expandable stents use cobalt-based and stainless-steel alloys. There are three types of stent cell structures: open-cell stents, closed-cell stents, and half-open cell stents. Generally, open-cell or half-open cell stents are more flexible than closed-cell stents (Fig. 2A-E).
There are two major methods to perform stent-assisted coiling: trans-cell coiling and jailed coiling. In trans-cell coiling, operators first release a stent to seal the neck of the aneurysm, then pass a microcatheter through the stent wall and insert the microcatheter into the aneurysm. In jailed coiling, operators first insert a microcatheter into the aneurysm, then release a stent to seal the neck of aneurysms and jail the microcatheter.
The use of stents remains controversial. Some studies claimed that stent-assisted coiling results in a significant decrease in angiographic recurrences [10,48]. However, one study showed no significant difference in long-term angiographic outcomes with or without stents [22]. The other problem is associated with complications. A study [48] showed that among patients treated by EVT with and without stents, the risks of permanent neurological procedure-related complications were 7.4% and 3.8%, respectively. Another study [59] indicated that stent-assisted coiling morbidity is higher than that of coiling without stents. In 2016, a meta-analysis that included 4,294 patients with aneurysms from 16 studies, showed that stent-assisted coiling has a higher long-term angiographic occlusion rate and a lower recurrence rate compared with those of coiling without stents [15]. Meanwhile, the rate of overall complications is not significantly different between the two methods, while ischemic strokes were more common in stent-assisted coiling. In 2019, a meta-analysis that included 1,408 patients with aneurysms from 8 studies indicated that there is a need of further research to determine if stent-assisted coiling increases the risk of unfavorable clinical outcomes [77].
Since the introduction of GDC into clinical practice, optimally releasing, and packing coils into complex aneurysms during the procedure, remain a problem. Stent-assisted coiling seems to be a proper method, but it remains an additional permanent device in the vessel, making patients take antiplatelet agents for a long time which brings a danger of extracranial bleeding during the period of dual antiplatelet therapy [21]. Furthermore, compared with balloon-assisted coiling, the stent structure with cells may more likely bring a danger of coil protrusion during procedures, leading to ischemic stroke [9].
In the neurointerventional field, the balloon was first used to treat a traumatic carotid-cavernous fistula [57]. Years after the appearance of GDC, operators started to use the balloon to assist coiling [31,42,43]. Before releasing coils, the balloon will be deployed in front of the aneurysm neck. It helps operators release and more efficiently pack coils into the aneurysm. Furthermore, operators can release more coils to improve the volumetric ratio without worrying about coil protrusion. After thorough packing of coils, operators remove the balloon to ensure that there is no device left in the vessel. The balloon can also be used as a rescue measure to remodel the coil once a coil protrusion happens [28] and to temporarily occlude the parent artery once the aneurysm ruptures during the procedure. Operators can perform better and reduce the time of the entire procedure with the assistance of the balloon in the treatment of complex aneurysms, which can decrease the risk of time-related complications. A cerebral vasospasm is a significant effect that leads to delayed cerebral ischemia and is a contributor to death after subarachnoid hemorrhage [35,61]. The balloon also plays a crucial role in the endovascular treatment of a cerebral vasospasm [23] (Fig. 2F).
In 2006, a study [60] that included 827 patients with intracranial aneurysms between 1995 and 2005, showed that balloon-assisted coiling has a significantly higher procedure-related complication rate than that of unassisted coiling (14.1% versus 3%) and that it has no improvement in the occlusion rate. However, a 2008 meta-analysis [58] showed that balloon-assisted coiling has no significant difference in thromboembolic events or iatrogenic ruptures with unassisted coiling and that it has a higher occlusion rate at initial and follow-up angiographic outcomes. Two studies [46,47] showed that for both ruptured and unruptured aneurysms, balloon-assisted coiling has a similar morbidity and mortality rates compared with those of unassisted coiling. One [46] of the two studies showed that balloon-assisted coiling has a relatively higher complete occlusion rate for ruptured aneurysms than that of unassisted coiling.
In 2016, a meta-analysis [70] that included 1,173 patients from 10 studies compared clinical outcomes of stentassisted coiling and balloon-assisted coiling. The two groups had no significant difference in the initial complete occlusion and retreatment rates. However, patients treated by stent-assisted coiling showed a higher complete occlusion rate at six months or later. Moreover, there was no significant difference in the procedure-related complication rates.
The appearance of flow diverter had overturned the traditional concept of intracranial aneurysms treatment. In 2001, the first use of overlapping stents to treat intracranial aneurysms without any coils, was reported [5]. It brought a possibility that intracranial aneurysms can be treated by changing hemodynamics though the absence of stuff packed into aneurysms. In 2007, the first intraluminal flow diverter device, the Pipeline Neuroendovascular Device, was applied to treat intracranial aneurysms [25] (Fig. 2G). Then, more types of devices were introduced into clinical practice.
Depending on their high level of metal coverage rate, flow diverters change the intra-aneurysmal hemodynamics. With the help of a flow diverter, more blood that initially flowed into aneurysms flows through the parent artery, and therefore, aneurysms will be gradually occluded due to flow stasis. Although traditional stents can also change the intra-aneurysmal hemodynamics [11,65], their effects on flow dynamics, including velocity vectors at the neck, maximum wall shear stress, inflow rate into the aneurysm, and turnover time, are significantly lower than those of a flow diverter [24]. Moreover, the flow diverter can promote thrombus formation in aneurysms due to its materials and its small mesh that allows platelet into aneurysms which hinders platelet from escaping [71]. Compared with traditional methods, the application of flow diverters has dramatically reduced difficulty and increased efficiency, especially in the treatment of giant aneurysms or other challenging aneurysms. Though the main character of flow diverters is more metal coverage, overlapping two flow diverters does not seem to be better than using one in aneurysmal flow reduction [13].
In 2013, a meta-analysis [6] that included 1,654 patients with aneurysms who were treated by flow diverter from 29 studies, showed that the complete occlusion rate was 76% for all aneurysms and 76% for giant aneurysms at six months. Furthermore, the procedure-related permanent morbidity rate was 5%, and the procedure-related mortality rate was 4%. In 2015, a retrospective study [26] that included 906 patients with aneurysms treated by flow diverter, showed a neurologic morbidity rate of 7.4% and a neurologic mortality rate of 3.8% (the median follow-up was 19.3 months). In 2019, a prospective cohort study [18] that included 477 patients with aneurysms treated by flow diverter, showed that the complete occlusion rate is 68.4% at 12 months, the permanent-related serious event rate is 5.9% and the mortality rate is 1.2%. Noteworthy, all three studies indicated that the complication rate is higher in the treatment of posterior circulation aneurysms and giant aneurysms.
The intraluminal flow diverter performs well in complex aneurysms, but its flow-diverting hemodynamic effect depends on the parent artery context. Once the parent artery context of the aneurysm is complex, including tortuous or bifurcated arteries, the intraluminal flow diverter may not work, and can even cause a procedurerelated ischemic stroke.
The flow diverter that was deployed within the aneurysm was designed to solve these problems. One typical intrasaccular flow diverter is the Woven EndoBridge device (WEB) (Fig. 2H). The WEB device has more metal coverage at the aneurysm neck (the coverage increases centripetally, ranging from 55% to 100%) [17], providing a higher level of hemodynamic effect. Moreover, WEB-treated patients do not require dual antiplatelet therapy.
A retrospective study [76] that included 48 patients with ruptured aneurysms and treated by WEB showed that the complete occlusion rate is 61.5%, the adequate occlusion rate is 92.3%, the recurrence rate is 38.5%, and the mortality rate is 6.3%. A systematic review [41] that included 377 patients with ruptured aneurysms from 9 studies concluded that the complete occlusion rate is 56.4%, the adequate occlusion rate is 84.8%, the retreatment rate is 4.5%, and the mortality rate is 13.6%. The two studies indicated that the risk of mortality is unneglectable in WEB-treated patients.
Though we can assess the effectiveness and safety of different treatments through various study outcomes, we also need to pay more attention to the characteristics of the intracranial aneurysm. These characteristics, such as aneurysm status (ruptured or not), and aneurysm location and morphology, also affect clinical outcomes, and operators will have to choose different methods according to the characteristics of the intracranial aneurysm. Furthermore, the experience of operators and perioperative management also plays a crucial role in the whole treatment procedure.
From neurosurgical clipping to endovascular coiling, endovascular coiling to stent-assisted or balloon-assisted coiling, and stent-assisted or balloon-assisted coiling to flow diversion treatment, patients with intracranial aneurysms have more opportunities to choose a more suitable strategy. Maybe, soon patients will not have to suffer rupture of intracranial aneurysms and face the risk of procedure-related complications.
REFERENCES
1. Algra AM, Lindgren A, Vergouwen MDI, Greving JP, van der Schaaf IC, van Doormaal TPC, et al. Procedural clinical complications, case-fatality risks, and risk factors in endovascular and neurosurgical treatment of unruptured intracranial aneurysms: A systematic review and meta-analysis. JAMA Neurol. 2019 Mar;76(3):282-93.



2. Backes D, Rinkel GJ, van der Schaaf IC, Nij Bijvank JA, Verweij BH, Visser-Meily JM, et al. Recovery to preinterventional functioning, return-to-work, and life satisfaction after treatment of unruptured aneurysms. Stroke. 2015 Jun;46(6):1607-12.


3. Barnett BP, Gailloud P. Assessment of EmboGelŌĆöA selectively dissolvable radiopaque hydrogel for embolic applications. J Vasc Interv Radiol. 2011 Feb;22(2):203-11.


4. Barnett BP, Hughes AH, Lin S, Arepally A, Gailloud PH. In vitro assessment of EmboGel and UltraGel radiopaque hydrogels for the endovascular treatment of aneurysms. J Vasc Interv Radiol. 2009 Apr;20(4):507-12.


5. Benndorf G, Herbon U, Sollmann WP, Campi A. Treatment of a ruptured dissecting vertebral artery aneurysm with double stent placement: Case report. AJNR Am J Neuroradiol. 2001 Nov-Dec;22(10):1844-8.


6. Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular treatment of intracranial aneurysms with flow diverters: A meta-analysis. Stroke. 2013 Feb;44(2):442-7.


7. Brinjikji W, Rabinstein AA, Nasr DM, Lanzino G, Kallmes DF, Cloft HJ. Better outcomes with treatment by coiling relative to clipping of unruptured intracranial aneurysms in the United States, 2001-2008. AJNR Am J Neuroradiol. 2011 JunJul;32(6):1071-5.



8. Broeders JA, Ahmed Ali U, Molyneux AJ, Poncyljusz W, Raymond J, White PM, et al. Bioactive versus bare platinum coils for the endovascular treatment of intracranial aneurysms: Systematic review and meta-analysis of randomized clinical trials. J Neurointerv Surg. 2016 Sep;8(9):898-908.


9. Cai K, Zhang Y, Shen L, Ni Y, Ji Q. Comparison of stent-assisted coiling and balloon-assisted coiling in the treatment of ruptured wide-necked intracranial aneurysms in the acute period. World Neurosurg. 2016 Dec;96:316-21.


10. Chalouhi N, Jabbour P, Gonzalez LF, Dumont AS, Rosenwasser R, Starke RM, et al. Safety and efficacy of endovascular treatment of basilar tip aneurysms by coiling with and without stent assistance: A review of 235 cases. Neurosurgery. 2012 Oct;71(4):785-94.

11. Cho SH, Jo WI, Jo YE, Yang KH, Park JC, Lee DH. Bench-top comparison of physical properties of 4 commercially-available self-expanding intracranial stents. Neurointervention. 2017 Mar;12(1):31-9.




12. Cloft HJ. Have you been smoking something that is biologically active? AJNR Am J Neuroradiol. 2006 Feb;27(2):240-2.


13. Damiano RJ, Tutino VM, Paliwal N, Ma D, Davies JM, Siddiqui AH, et al. Compacting a single flow diverter versus overlapping flow diverters for intracranial aneurysms: A computational study. AJNR Am J Neuroradiol. 2017 Mar;38(3):603-10.



14. Etminan N, Rinkel GJ. Unruptured intracranial aneurysms: Development, rupture and preventive management. Nat Rev Neurol. 2016 Dec;12(12):699-713.



15. Feng MT, Wen WL, Feng ZZ, Fang YB, Liu JM, Huang QH. Endovascular embolization of intracranial aneurysms: To use stent(s) or not? Systematic review and meta-analysis. World Neurosurg. 2016 Sep;93:271-8.


16. Fessler RD, Ringer AJ, Qureshi AI, Guterman LR, Hopkins LN. Intracranial stent placement to trap an extruded coil during endovascular aneurysm treatment: Technical note. Neurosurgery. 2000 Jan;46(1):248-51; discussion 251-3.


17. Fiorella D, Molyneux A, Coon A, Szikora I, Saatci I, Baltacioglu F, et al. Demographic, procedural and 30-day safety results from the WEB Intra-saccular Therapy Study (WEBIT). J Neurointerv Surg. 2017 Dec;9(12):1191-6.


18. Gory B, Berge J, Bonaf├® A, Pierot L, Spelle L, Piotin M, et al. Flow diverters for intracranial aneurysms: The DIVERSION National Prospective Cohort Study. Stroke. 2019 Dec;50(12):3471-80.

19. Greving JP, Wermer MJ, Brown RD Jr, Morita A, Juvela S, Yonekura M, et al. Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: A pooled analysis of six prospective cohort studies. Lancet Neurol. 2014 Jan;13(1):59-66.


20. Guglielmi G, Vi├▒uela F, Dion J, Duckwiler G. Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: Preliminary clinical experience. J Neurosurg. 1991 Jul;75(1):8-14.

21. Hao Q, Tampi M, OŌĆÖDonnell M, Foroutan F, Siemieniuk RA, Guyatt G. Clopidogrel plus aspirin versus aspirin alone for acute minor ischaemic stroke or high risk transient ischaemic attack: Systematic review and meta-analysis. BMJ. 2018 Dec;363:k5108.



22. Hwang G, Park H, Bang JS, Jin SC, Kim BC, Oh CW, et al. Comparison of 2-year angiographic outcomes of stent- and nonstent-assisted coil embolization in unruptured aneurysms with an unfavorable configuration for coiling. AJNR Am J Neuroradiol. 2011 Oct;32(9):1707-10.



23. Jabbarli R, Pierscianek D, R├Člz R, Darkwah Oppong M, Kaier K, Shah M, et al. Endovascular treatment of cerebral vasospasm after subarachnoid hemorrhage: More is more. Neurology. 2019 Jul;93(5):e458-66.

24. Jankowitz BT, Gross BA, Seshadhri S, Girdhar G, Jadhav A, Jovin TG, et al. Hemodynamic differences between Pipeline and coil-adjunctive intracranial stents. J Neurointerv Surg. 2019 Sep;11(9):908-11.


25. Kallmes DF, Ding YH, Dai D, Kadirvel R, Lewis DA, Cloft HJ. A new endoluminal, flow-disrupting device for treatment of saccular aneurysms. Stroke. 2007 Aug;38(8):2346-52.


26. Kallmes DF, Hanel R, Lopes D, Boccardi E, Bonaf├® A, Cekirge S, et al. International retrospective study of the pipeline embolization device: A multicenter aneurysm treatment study. AJNR Am J Neuroradiol. 2015 Jan;36(1):108-15.


27. Kim S, Nowicki KW, Gross BA, Wagner WR. Injectable hydrogels for vascular embolization and cell delivery: The potential for advances in cerebral aneurysm treatment. Biomaterials. 2021 Oct;277:121109.


28. Ko HC. Rescue balloon-assisted remodeling technique for protrusion of coil loop: A case report. Medicine (Baltimore). 2021 May;100(19):e25783.


29. Komotar RJ, Mocco J, Solomon RA. Guidelines for the surgical treatment of unruptured intracranial aneurysms: The first annual J. Lawrence pool memorial research symposium -controversies in the management of cerebral aneurysms. Neurosurgery. 2008 Jan;62(1):183-93; discussion 193-4.

30. Kotowski M, Naggara O, Darsaut TE, Nolet S, Gevry G, Kouznetsov E, et al. Safety and occlusion rates of surgical treatment of unruptured intracranial aneurysms: A systematic review and meta-analysis of the literature from 1990 to 2011. J Neurol Neurosurg Psychiatry. 2013 Jan;84(1):42-8.


32. Li H, Pan R, Wang H, Rong X, Yin Z, Milgrom DP, et al. Clipping versus coiling for ruptured intracranial aneurysms: A systematic review and meta-analysis. Stroke. 2013 Jan;44(1):29-37.


33. Lindgren A, Vergouwen MD, van der Schaaf I, Algra A, Wermer M, Clarke MJ, et al. Endovascular coiling versus neurosurgical clipping for people with aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2018 Aug;8(8):CD003085.


34. Luther E, McCarthy DJ, Brunet MC, Sur S, Chen SH, Sheinberg D, et al. Treatment and diagnosis of cerebral aneurysms in the post-International Subarachnoid Aneurysm Trial (ISAT) era: Trends and outcomes. J Neurointerv Surg. 2020 Jul;12(7):682-7.


35. Macdonald RL. Delayed neurological deterioration after subarachnoid haemorrhage. Nat Rev Neurol. 2014 Jan;10(1):44-58.



36. McDougall CG, Johnston SC, Hetts SW, Gholkar A, Barnwell SL, Vazquez Suarez JC, et al. Five-year results of randomized bioactive versus bare metal coils in the treatment of intracranial aneurysms: The Matrix and Platinum Science (MAPS) Trial. J Neurointerv Surg. 2021 Oct;13(10):930-4.


37. Moftakhar R, Xu F, Aagaard-Kienitz B, Consigny DW, Grinde JR, Hart K, et al. Preliminary in vivo evaluation of a novel intrasaccular cerebral aneurysm occlusion device. J Neurointerv Surg. 2015 Aug;7(8):584-90.


38. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised trial. Lancet. 2002 Oct;360(9342):1267-74.


39. Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT). Lancet. 2015 Feb;385(9969):691-7.



40. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005 Sep;366(9488):809-17.


41. Monteiro A, Lazar AL, Waqas M, Rai HH, Baig AA, Cortez GM, et al. Treatment of ruptured intracranial aneurysms with the Woven EndoBridge device: A systematic review. J Neurointerv Surg. 2022 Apr;14(4):366-70.


42. Moret J, Cognard C, Weill A, Castaings L, Rey A. The ŌĆ£remodelling techniqueŌĆØ in the treatment of wide neck intracranial aneurysms. Angiographic results and clinical follow-up in 56 cases. Interv Neuroradiol. 1997 Mar;3(1):21-35.



43. Moret J, Pierot L, Boolin A. Remodelling of the arterial wall of the parent vessel in the endovascular treatment of intracranial aneurysms. Neuroradiology. 1994 36(Suppl 1):S83.
44. Naggara ON, White PM, Guilbert F, Roy D, Weill A, Raymond J. Endovascular treatment of intracranial unruptured aneurysms: Systematic review and meta-analysis of the literature on safety and efficacy. Radiology. 2010 Sep;256(3):887-97.


45. Nieuwkamp DJ, Setz LE, Algra A, Linn FH, de Rooij NK, Rinkel GJ. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol. 2009 Jul;8(7):635-42.


46. Pierot L, Cognard C, Anxionnat R, Ricolfi F; CLARITY Investigators. Remodeling technique for endovascular treatment of ruptured intracranial aneurysms had a higher rate of adequate postoperative occlusion than did conventional coil embolization with comparable safety. Radiology. 2011 Feb;258(2):546-53.


47. Pierot L, Spelle L, Leclerc X, Cognard C, Bonaf├® A, Moret J. Endovascular treatment of unruptured intracranial aneurysms: Comparison of safety of remodeling technique and standard treatment with coils. Radiology. 2009 Jun;251(3):846-55.


48. Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, et al. Stent-assisted coiling of intracranial aneurysms: Clinical and angiographic results in 216 consecutive aneurysms. Stroke. 2010 Jan;41(1):110-5.


49. Piotin M, Mandai S, Murphy KJ, Sugiu K, Gailloud P, Martin JB, et al. Dense packing of cerebral aneurysms: An in vitro study with detachable platinum coils. AJNR Am J Neuroradiol. 2000 Apr;21(4):757-60.


50. Poupart O, Conti R, Schmocker A, Pancaldi L, Moser C, Nuss KM, et al. Pulsatile flow-induced fatigue-resistant photopolymerizable hydrogels for the treatment of intracranial aneurysms. Front Bioeng Biotechnol. 2021 Jan;8:619858.



51. Poupart O, Schmocker A, Conti R, Moser C, Nuss KM, Gr├╝tzmacher H, et al. In vitro implementation of photopolymerizable hydrogels as a potential treatment of intracranial aneurysms. Front Bioeng Biotechnol. 2020 Apr;8:261.



52. Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003 Jun;34(6):1398-403.


53. Raymond J, Guilbert F, Weill A, Roy D, LeBlanc P, G├®vry G, et al. Safety, science, and sales: A request for valid clinical trials to assess new devices for endovascular treatment of intracranial aneurysms. AJNR Am J Neuroradiol. 2004 Aug;25(7):1128-30.


54. Rezek I, Mousan G, Wang Z, Murad MH, Kallmes DF. Coil type does not affect angiographic follow-up outcomes of cerebral aneurysm coiling: A systematic review and meta-analysis. AJNR Am J Neuroradiol. 2013 Sep;34(9):1769-73.



55. Rezek I, Mousan G, Wang Z, Murad MH, Kallmes DF. Effect of core laboratory and multiple-reader interpretation of angiographic images on follow-up outcomes of coiled cerebral aneurysms: A systematic review and meta-analysis. AJNR Am J Neuroradiol. 2013 Jul;34(7):1380-4.



56. Roquer J, Cuadrado-Godia E, Guimaraens L, Conesa G, Rodr├Łguez-Campello A, Capellades J, et al. Short- and long-term outcome of patients with aneurysmal subarachnoid hemorrhage. Neurology. 2020 Sep;95(13):e1819-29.



57. Serbinenko FA. Okkliuziia ballonom kavernoznogo otdels sonno─Ł arterii kak metod lecheniia karotidno-kavernoznykh sousti─Ł [Occlusion of the cavernous portion of the carotid artery with a balloon as a method of treating carotid-cavernous anastomosis]. Vopr Neirokhir. 1971 Nov-Dec;35(6):3-9.
58. Shapiro M, Babb J, Becske T, Nelson PK. Safety and efficacy of adjunctive balloon remodeling during endovascular treatment of intracranial aneurysms: A literature review. AJNR Am J Neuroradiol. 2008 Oct;29(9):1777-81.



59. Shapiro M, Becske T, Sahlein D, Babb J, Nelson PK. Stent-supported aneurysm coiling: A literature survey of treatment and follow-up. AJNR Am J Neuroradiol. 2012 Jan;33(1):159-63.



60. Sluzewski M, van Rooij WJ, Beute GN, Nijssen PC. Balloon-assisted coil embolization of intracranial aneurysms: Incidence, complications, and angiography results. J Neurosurg. 2006 Sep;105(3):396-9.

61. Solenski NJ, Haley EC Jr, Kassell NF, Kongable G, Germanson T, Truskowski L, et al. Medical complications of aneurysmal subarachnoid hemorrhage: A report of the multicenter, cooperative aneurysm study. Participants of the Multicenter Cooperative Aneurysm Study. Crit Care Med. 1995 Jun;23(6):1007-17.

62. Takao H, Murayama Y, Saguchi T, Ishibashi T, Ebara M, Irie K, et al. Endovascular treatment of experimental cerebral aneurysms using thermoreversible liquid embolic agents. Interv Neuroradiol. 2006 Jan;12(Suppl 1):154-7.




63. Takigawa T, Matsumaru Y, Nakai Y, Nakamura K, Hayakawa M, Tsuruta W, et al. Bioactive coils cause headache and fever after endovascular treatment of intracranial aneurysms. Headache. 2012 Feb;52(2):312-21.


64. Tamatani S, Ito Y, Abe H, Koike T, Takeuchi S, Tanaka R. Evaluation of the stability of aneurysms after embolization using detachable coils: Correlation between stability of aneurysms and embolized volume of aneurysms. AJNR Am J Neuroradiol. 2002 May;23(5):762-7.


65. Tateshima S, Tanishita K, Hakata Y, Tanoue SY, Vi├▒uela F. Alteration of intraaneurysmal hemodynamics by placement of a self-expandable stent. Laboratory investigation. J Neurosurg. 2009 Jul;111(1):22-7.

66. Thornton J, Debrun GM, Aletich VA, Bashir Q, Charbel FT, Ausman J. Follow-up angiography of intracranial aneurysms treated with endovascular placement of Guglielmi detachable coils. Neurosurgery. 2002 Feb;50(2):239-49; discussion 249-50.


67. Uchiyama N, Kida S, Nomura M, Hasegawa M, Yamashima T, Yamashita J, et al. Significance of volume embolization ratio as a predictor of recanalization on endovascular treatment of cerebral aneurysms with guglielmi detachable coils. Interv Neuroradiol. 2000 Nov;6 Suppl 1(Suppl 1):59-63.



68. van Rooij WJ, de Gast AN, Sluzewski M. Results of 101 aneurysms treated with polyglycolic/polylactic acid microfilament nexus coils compared with historical controls treated with standard coils. AJNR Am J Neuroradiol. 2008 May;29(5):991-6.



69. Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis. Lancet Neurol. 2011 Jul;10(7):626-36.


70. Wang F, Chen X, Wang Y, Bai P, Wang HZ, Sun T, et al. Stent-assisted coiling and balloon-assisted coiling in the management of intracranial aneurysms: A systematic review & meta-analysis. J Neurol Sci. 2016 May;364:160-6.


71. Wang K, Huang Q, Hong B, Li Z, Fang X, Liu J. Correlation of aneurysm occlusion with actual metal coverage at neck after implantation of flow-diverting stent in rabbit models. Neuroradiology. 2012 Jun;54(6):607-13.



72. White PM, Lewis SC, Gholkar A, Sellar RJ, Nahser H, Cognard C, et al. Hydrogel-coated coils versus bare platinum coils for the endovascular treatment of intracranial aneurysms (HELPS): A randomised controlled trial. Lancet. 2011 May;377(9778):1655-62.


73. White PM, Lewis SC, Nahser H, Sellar RJ, Goddard T, Gholkar A. HydroCoil Endovascular Aneurysm Occlusion and Packing Study (HELPS trial): Procedural safety and operator-assessed efficacy results. AJNR Am J Neuroradiol. 2008 Feb;29(2):217-23.



74. White PM, Raymond J. Endovascular coiling of cerebral aneurysms using ŌĆ£bioactiveŌĆØ or coated-coil technologies: A systematic review of the literature. AJNR Am J Neuroradiol. 2009 Feb;30(2):219-26.



75. Wiebers DO, Piepgras DG, Meyer FB, Kallmes DF, Meissner I, Atkinson JL, et al. Pathogenesis, natural history, and treatment of unruptured intracranial aneurysms. Mayo Clin Proc. 2004 Dec;79(12):1572-83.


76. Youssef PP, Dornbos D III, Peterson J, Sweid A, Zakeri A, Nimjee SM, et al. Woven EndoBridge (WEB) device in the treatment of ruptured aneurysms. J Neurointerv Surg. 2021 May;13(5):443-6.


-
METRICS

-
- 0 Crossref
- 0 Scopus
- 443 View
- 14 Download
- ORCID iDs
-
Dongming Liang

https://orcid.org/0000-0002-7077-5747 - Related articles
-
ERRATUM: Endovascular treatment of ruptured tiny aneurysms2023 December;25(4)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



