 |
 |
| J Cerebrovasc Endovasc Neurosurg > Volume 25(4); 2023 > Article |
|
Abstract
Craniotomy is known as a cause of iatrogenic dural cerebral arteriovenous fistula (AVF). However, mixed pial and dural AVFs after craniotomy are extremely rare and require accurate diagnosis and prompt treatment due to their aggressiveness. We present a case of an iatrogenic mixed pial and dural AVF diagnosed 2 years after pterional craniotomy for surgical clipping of a ruptured anterior choroidal aneurysm. The lesion was successfully treated using single endovascular procedure of transvenous coil embolization through the engorged vein of Labbe and the superficial middle cerebral vein. The possibility of the AVF formation after the pterional approach should always be kept in mind because it usually occurs at the middle cranial fossa, which frequently has an aggressive nature owing to direct cortical venous or leptomeningeal drainage patterns. This complication is believed to be caused by angiogenetic conditions due to coagulation, retraction, and microinjuries of the perisylvian vessels, and can be prevented by performing careful sylvian dissection according to patient-specific perisylvian venous anatomy.
Cerebral arteriovenous fistula (AVF) is a rare heterogeneous vascular disease that has various morphological and hemodynamical differences of draining veins and feeding arteries among cases [7,10,18,22,25]. Dural AVFs are defined as AVFs fed by branches of the dural arteries and are lesions occasionally associated with cerebral venous thrombosis, inflammation, trauma, and craniotomy. On the other hand, pial AVFs consist of feeders from the pial arteries, which are related to congenital and various conditions, such as Ehlers-Danlos syndrome and neurofibromatosis type 1 [2,6,7,18]. Due to the differences in etiology, mixed dural and pial AVF is an extremely rare condition, which has been infrequently reported worldwide [6].
Some reports have described iatrogenic AVF after various craniotomies, and intraoperative microinjuries, venous thrombosis, and sinus occlusions are known pathophysiologies [1,4-6,9,10,14,20,25,28,29]. However, AVF formation after aneurysm surgery through the pterional approach is infrequently reported despite the large number of the surgeries worldwide [4,6,25]. Although the disease may result in fatal neurological outcomes due to venous hypertension and intracranial hemorrhage, it may be overlooked or missed if asymptomatic, as iatrogenic AVF is not a well-known complication of clipping surgery.
We present an extremely rare case of mixed pial and dural AVF at the middle cranial fossa after a conventional pterional approach for surgical clipping of a ruptured anterior choroidal artery aneurysm which was successfully treated with endovascular transvenous embolization through the engorged vein of Labbe.
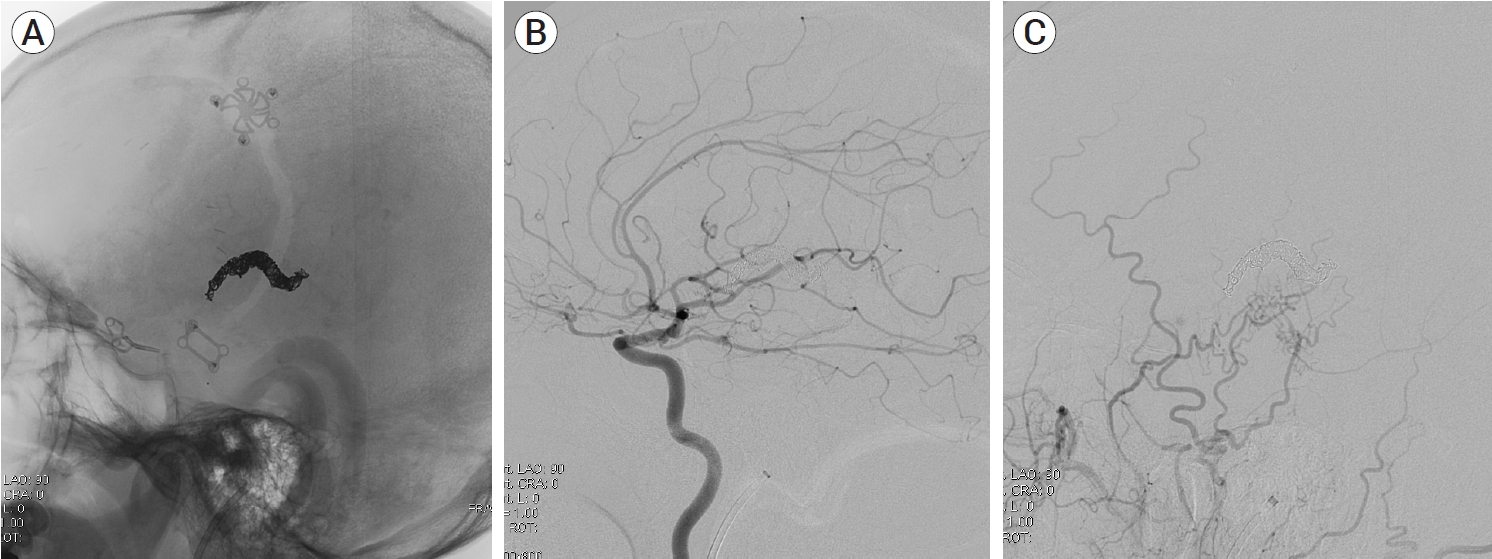
A 39-year-old man visited the neurosurgery department and presented with a left-sided pulsatile headache. The patient had a history of surgical clipping for a ruptured left anterior choroidal artery aneurysm using a conventional pterional approach 2 years previously. Computed tomography (CT) angiography revealed engorged tortuous cortical vessels near the previous craniotomy site and sylvian fissure, indicating a suspicious AVF which had not been detected on CT conducted 2-years before presentation (Fig. 1). Digital subtraction angiography (DSA) was performed for treatment planning, and external carotid angiography demonstrated a dural AVF fed by the branches of the middle meningeal artery (MMA) and superficial temporal artery (STA), draining directly into the engorged superficial middle cerebral vein (SMCV), vein of Labbe, and sigmoid sinus (Fig. 2A). Ectatic changes in the draining veins and cortical venous reflux were observed. Ipsilateral internal carotid artery angiography revealed additional multiple feeders arising from the middle cerebral artery (MCA), suggesting a mixed pial and dural AVF (Fig. 2B, C). Due to the difficulty of the transarterial approach through multiple small feeding arteries, transvenous coil embolization was performed via the sigmoid sinus and enlarged vein of Labbe (Fig. 3). Complete obliteration of the fistula was achieved, confirmed by postoperative DSA (Fig. 4), and the patient was discharged with no neurological complications.
Development of an acquired dural AVF, and the associated pathophysiology, has two main reported hypotheses. The first is related to progressive venous sinus thrombosis and the opening of microvascular connections. The sinus thrombosis or occlusion occurring during posterior fossa and midline craniotomy surgery may therefore trigger iatrogenic dural AVF [20,22,28,29]. The second mechanism of dural AVF development is the expression of angiogenesis growth factors due to a neovascularization-promoting environment such as inflammation, ischemia, hemorrhage, and traumatic vessel injuries [3,6,16]. Craniotomy is the most common cause of iatrogenic dural AVF formation, but the mechanism of the pathology remains unknown; however, the leading hypothesis is that inflammatory reactions and the repair processes of intraoperative injuries are responsible for the pathophysiology, which is related to second hypothesis of dural AVF formation explained above [4-6,9,13,14]. Many reports have proven that angioneogenesis is caused by the release of vascular endothelial growth factor after traumatic vessel injuries and parenchymal injury, and this explains and supports the mechanism of AVF formation after vascular microinjury during craniotomy and brain dissections [3,6,16]. Incomplete dural closure also may be a cause of abnormal epidural and intradural anastomosis and angiogenetic environment.
Unlike dural AVFs, which are mostly acquired lesions consisting of dural arterial feeders, pial AVFs are fed by pial arterial branches or cortical arteries and are generally associated with younger patients and congenital diseases such as Ehlers-Danlos syndrome, Rendu-OilerWeber disease, and neurofibromatosis type 1 [2,6,7,18,19,21]. Iatrogenic pial AVF is a rarer condition, and there have been some reports of acquired pial AVFs after numerous procedures such as craniotomy and radiosurgery, or repeated trauma [2,6,18]. Pial AVF requires prompt treatment because the high flow of the fistula makes it more aggressive than dural AVFs and more often creates venous ectasia [2,7,15,26]. Furthermore, they usually have multiple small arterial feeders from pial or cortical arteries, which complicates treatment [7,26].
Because of the difference in etiology between pial AVF and dural AVF, mixed pial and dural AVF is very rarely reported. To the best of our knowledge, the present case is the first of a directly diagnosed mixed pial and dural AVF after craniotomy that has demonstrated prominent pial arterial feeders from the MCA and dural arterial feeders from the MMA and STA. The drainage pattern of the AVF via the SMCV and the engorged anastomotic vein of Labbe enabled us to approach transvenously via the sigmoid sinus and perform successful coil embolization of the fistulous points. The transarterial approach and open surgery were not attempted because the fistula had multiple small tortuous pial arterial feeders arising from the MCA branches and dural arterial feeders arising from the MMA and STA.
Doi et al. (2019) reported a late diagnosed mixed pial and dural AVF after craniotomy [6]. Postoperative DSA after open surgery for an iatrogenic dural AVF caused by surgical clipping of an MCA aneurysm showed complete obliteration of the dural feeders. However, it also revealed remnant fistula and new feeders from multiple pial arterial branches near a previously clipped aneurysm, indicating the AVF was a mixed pial and dural AVF. Preoperative DSA showed only dural arterial feeders from the MMA and did not show feeders from the pial arteries, which misled the authors to consider it a dural AVF. The high flow of dural arterial feeders may have blocked the flow of the small pial arterial feeders preoperatively. Additional gamma knife surgery was performed for obliteration of the remnant fistula [6].
Although a greater number of patients undergo aneurysm surgery worldwide through the pterional approach than other craniotomies, few reports of iatrogenic AVF following the procedure have been published [4,6,25]. Sylvian fissure dissection is performed during most surgeries for anterior circulation artery aneurysms; therefore, manipulation, coagulation, and retraction of perisylvian vessels may be potential causes of AVF formation. Consequently, the surgeon should take care, as much as is possible, that such vessels are not damaged during sylvian fissure dissection [17]. The SMCV can interfere with the pterional approach; therefore, good knowledge of the various anatomical relationships between the SMCV and the frontotemporal lobe is required. According to Yasargil (1984), vascular neurosurgeons tend to dissect between the SMCV and frontal lobe during the transsylvian approach [27]. However, this may lead to unnecessary manipulation and coagulation of the fronto-sylvian bridging veins [11,12,17]. Imada et al. (2021, 2019) used cadaver dissection to understand and introduce morphological patterns and classification of the SMCV based on its relationship with fronto-sylvian and temporo-sylvian veins, which is a useful reference during surgery [11,12]. Unnecessary damage can be prevented by performing sylvian dissection according to the patient’s specific SMCV anatomy.
Anatomically, iatrogenic AVF after the transsylvian approach occurs at the middle cranial fossa, which usually has a venous drainage pattern involving the sphenoparietal, sphenopetrous, or sphenobasilar sinuses. Moreover, they occasionally drain directly through cortical veins or leptomeningeal veins, which results in more aggressive behavior than AVFs at other locations [7,8,23,24]. Therefore, the possibility of the AVF formation after the pterional approach should always be kept in mind and not be missed. Our case also showed middle cranial fossa AVF draining directly via SMCV, not the venous sinuses, which presented high-grade AVF leading to venous hypertension. Although it did not show intracranial hemorrhage, it was promptly treated because of its aggressiveness and patient symptoms.
We present an extremely rare case of iatrogenic mixed pial and dural AVF that occurred after surgical clipping of a ruptured anterior choroidal artery aneurysm, which was successfully treated using an endovascular transvenous approach. AVFs acquired after the pterional approach usually occur in the middle cranial fossa and should be well recognized and promptly treated owing to their aggressiveness. Neurosurgeons should perform careful sylvian fissure dissection based on the patient-specific venous anatomy, since angioneogenesis after manipulation, retraction, and coagulation of nearby vessels may be a potential cause of iatrogenic AVF formation.
Fig. 1.
(A) Contrast-enhanced computed tomography (CT) scan showing venous ectasias beneath the previous left craniotomy site (black arrow). (B) Three-dimensionally reconstructed CT angiography demonstrating suspicious dual arteriovenous fistula with multiple feeders from pial arteries (black arrow) and dural arteries (white arrow). Cortical venous reflux and venous hypertension is suspected (arrowhead).
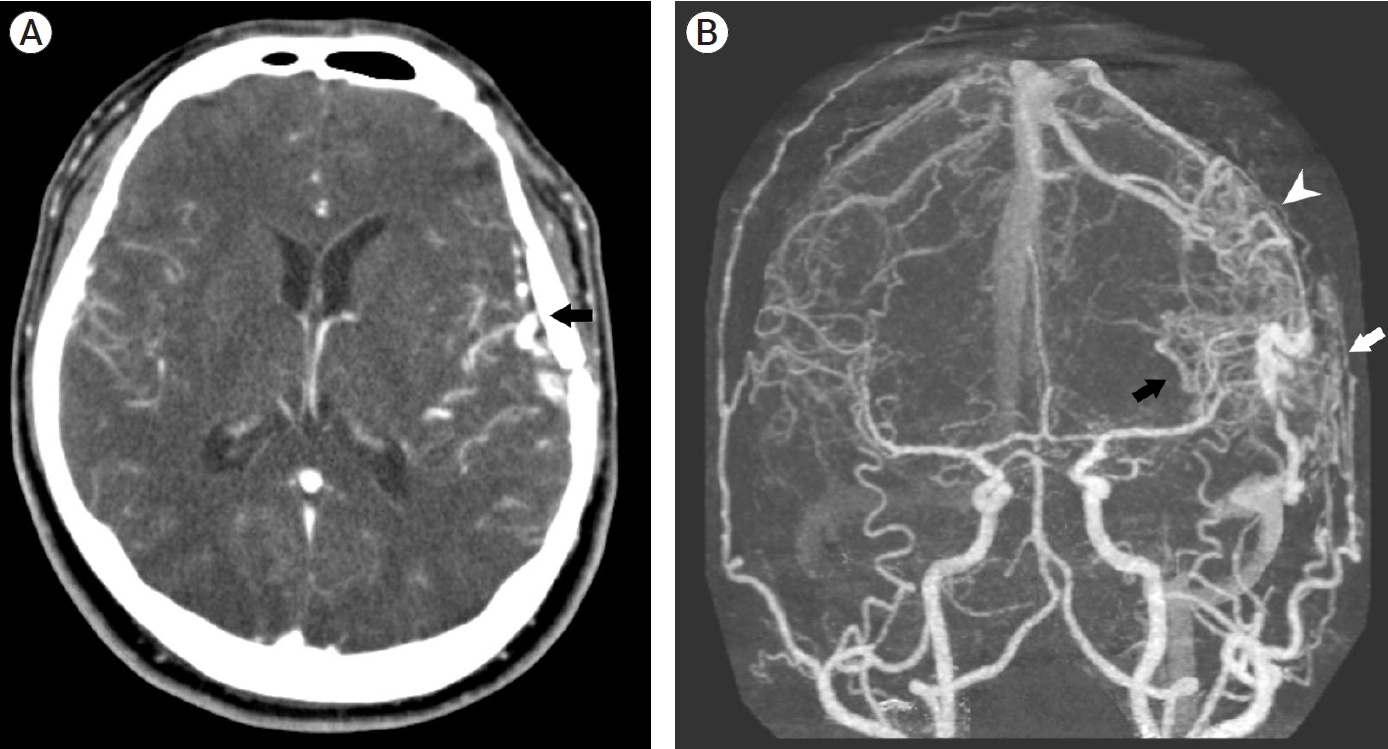
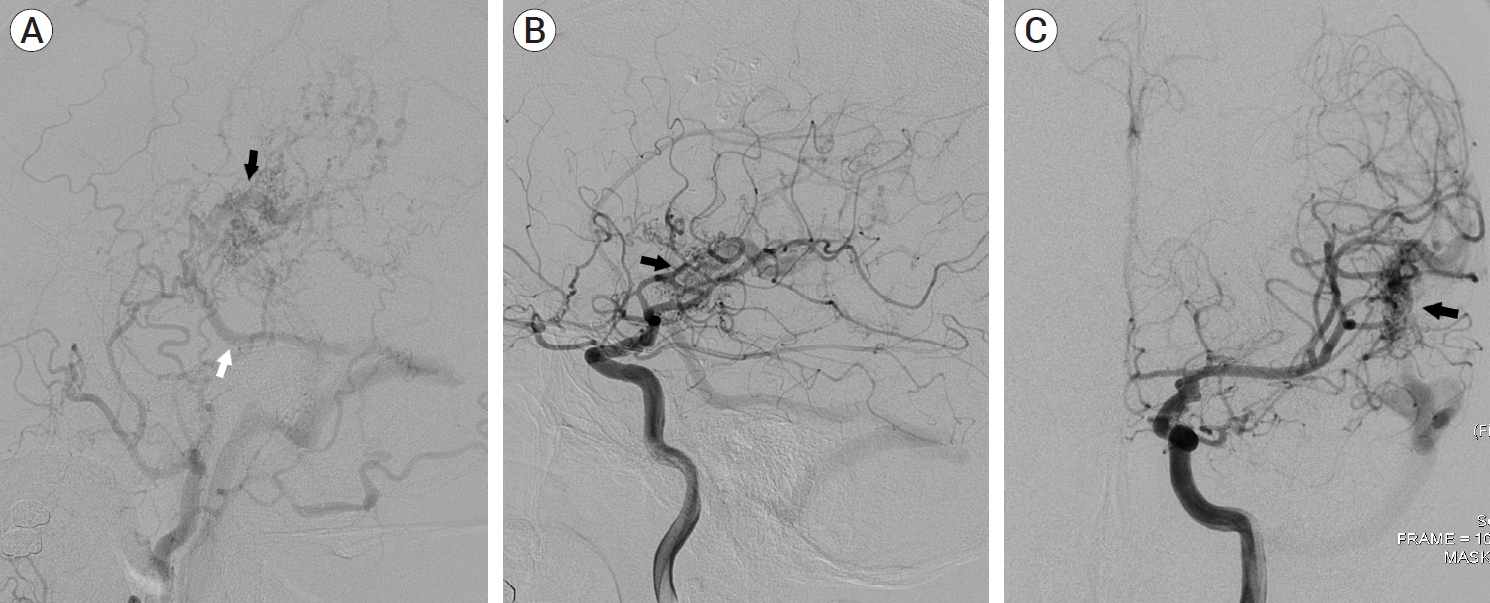
Fig. 2.
(A) Left external carotid artery angiography demonstrating multiple feeders from the middle meningeal artery and superficial temporal artery. Drainage pattern to engorge the superficial middle cerebral vein (black arrow) and vein of Labbe (white arrow) is noted. (B, C) Left internal carotid artery angiography showing additional multiple pial arterial feeders arising from the middle cerebral artery (black arrow).
REFERENCES
1. Ahn JY, Kim OJ, Joo YJ, Joo JY. Dural arteriovenous malformation occurring after craniotomy for pial arteriovenous malformation. J Clin Neurosci. 2003 Jan;10(1):134-6.


2. Atsushi S, Mikawa S, Akamatsu Y, Saito H, Seki H. A case of multiple pial arteriovenous fistulas associated with dural arteriovenous fistula. J Neurosurg. 2008 Dec;109(6):1103-7.


3. Bhogal P, Yeo LL, Henkes H, Krings T, Soderman M. The role of angiogenesis in dural arteriovenous fistulae: The story so far. Interv Neuroradiol. 2018 Aug;24(4):450-4.




4. Demartini Z Jr, Laurenti M, Oliveira T, Koppe G, Santos M, Francisco A. Postoperative dural arteriovenous fistula after clipping of ruptured saccular aneurysm of pericallosal artery. Arq Bras Neurocir. 2016 35(3):248-52.

5. Ding D, Brew S, McGuinness B, Mee EW. Iatrogenic dural arteriovenous fistula after surgical resection of a ruptured brain arteriovenous malformation. J Neurosci Rural Pract. 2016 Oct-Dec;7(4):604-6.



6. Doi K, Otani N, Hayashi M, Takeuchi S, Toyooka T, Wada K. Mixed pial and dural arteriovenous fistula after craniotomy: Case report and literature review. Br J Neurosurg. 2019 Oct;1-4.

7. Funakoshi Y, Hatano T, Saka M, Ando M, Chihara H, Takita W, et al. Dural and pial arteriovenous fistulas connected to the same drainer in the middle cranial fossa: A case report. World Neurosurg. 2018 Oct;118:47-52.


9. Higashida T. Delayed postoperative dural arteriovenous fistula presenting with progressive dementia. BMJ Case Rep. 2015 Dec;2015:bcr2015212874.



10. Huang MC, Wang YC, Huang JS, Huang KM. Postoperative developmental dural arteriovenous fistula. Formosan Journal of Surgery. 2015 48(3):102-6.

11. Imada Y, Kurisu K, Takumi T, Aoyama H, Sadatomo T, Migita K, et al. Morphological pattern and classification of the superficial middle cerebral vein by cadaver dissections: An embryological viewpoint. Neurol Med Chir (Tokyo). 2019 Jul;59(7):264-70.



12. Imada Y, Mihara C, Kawamoto H, Kurisu K. Dissection of the sylvian fissure in the trans-sylvian approach based on the morphological classification of the superficial middle cerebral vein. Neurol Med Chir (Tokyo). 2021 Dec;61(12):731-40.



13. Kanematsu R, Hanakita J, Takahashi T, Tomita Y, Minami M. An acquired cervical dural arteriovenous fistula after cervical anterior fusion: Case report and literature review. World Neurosurg. 2019 Aug;128:50-4.


14. Kim SW, Chae KS, Shim JH, Rho SJ, Choi HK, Park HS. Iatrogenic dural arteriovenous fistula after superficial temporal artery to middle cerebral artery anastomosis: A case report. Korean J Neurotrauma. 2015 Oct;11(2):151-3.



15. Lee JY, Son YJ, Kim JE. Intracranial pial arteriovenous fistulas. J Korean Neurosurg Soc. 2008 Aug;44(2):101-4.



16. Li Q, Zhang Q, Huang QH, Fang YB, Zhang ZL, Xu Y, et al. A pivotal role of the vascular endothelial growth factor signaling pathway in the formation of venous hypertension-induced dural arteriovenous fistulas. Mol Med Rep. 2014 May;9(5):1551-8.



17. Maekawa H, Hadeishi H. Venous-preserving sylvian dissection. World Neurosurg. 2015 84(6):2043-52.


18. Nishiyama Y, Kanemaru K, Yoshioka H, Hanihara M, Horikoshi T, Kniouchi H. Intracranial pial arteriovenous fistula caused by dural tenting: Case report. Neurol Med Chir (Tokyo). 2014 54(3):242-4.



19. Osada T, Krings T. Intracranial dural arteriovenous fistulas with pial arterial supply. Neurosurgery. 2019 Jan;84(1):104-15.


20. Pabaney AH, Robin AM, Basheer A, Malik G. Surgical management of dural arteriovenous fistula after craniotomy: Case report and review of literature. World Neurosurg. 2016 May;89:731.

21. Paramasivam S, Toma N, Niimi Y, Berenstein A. Development, clinical presentation and endovascular management of congenital intracranial pial arteriovenous fistulas. J Neurointerv Surg. 2013 May;5(3):184-90.


22. Park JS, Lee JM. Acquired dural arteriovenous fistula after cerebellopontine angle meningioma: A case report. Medicine (Baltimore). 2022 Jul;101(28):e29671.


23. Shimizu Y, Tokuda K, Park C. Sphenoid wing dural arteriovenous fistula: A case report and literature review. Surg Neurol Int. 2020 Dec;11:438.



24. Tanaka T, Kato N, Arai T, Hasegawa Y, Abe T. Surgical treatment of a sylvian-middle fossa dural arteriovenous fistula draining into the basal vein of rosenthal with frontotemporal craniotomy. J Stroke Cerebrovasc Dis. 2012 May;21(4):333-7.


25. Vadivelu S, Xin X, Loven T, Restrepo G, Chalif DJ, Setton A. Iatrogenic dural arteriovenous fistula and aneurysmal subarachnoid hemorrhage. Neurosurg Focus. 2012 May;32(5):e1.

26. Yamashita K, Ohe N, Yochimura S, Iwama T. Intracranial pial arteriovenous fistula. Neurol Med Chir (Tokyo). 2007 Dec;47(12):550-4.

27. Yasargil MG. Microneurosurgery. NewYork: Georg Thieme Verlag; 1984. p. 5-168, 215-33.
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,183 View
- 31 Download
- ORCID iDs
-
Chang-Young Lee

https://orcid.org/0000-0001-6046-2571 - Related articles




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



