 |
 |
| J Cerebrovasc Endovasc Neurosurg > Epub ahead of print |
Abstract
While mechanical thrombectomy is known to be effective for distal medium vessel occlusion (DMVO) as well as large vessel occlusion, tortuous DMVO are predisposed to vessel injury during stent retriever thrombectomy. Furthermore, getting access to the thrombus may be difficult during suction thrombectomy using a dedicated suction catheter. Most studies describe DMVO treatment using stent retrievers and dedicated suction catheters, but there are limited studies reporting DMVO treated with suction thrombectomy using a microcatheter. Herein, we describe three cases of DMVO treated with suction thrombectomy that was performed using a microcatheter and subsequently showed good results. Therefore, suction thrombectomy using a microcatheter is a viable alternative treatment for tortuous DMVO.
The effectiveness of mechanical thrombectomy for large-vessel occlusion has been demonstrated in several randomized clinical trials [1,2,7,12,20]. Several studies have reported the usefulness of mechanical thrombectomy for distal medium vessel occlusion (DMVO), including middle cerebral artery (MCA) M2 segment, using a dedicated suction catheter such as 3MAX or 4MAX (Penumbra, Alameda, CA, USA), or a stent retriever [6,10,11,15,16,18,19,22].
However, hemorrhagic complications are relatively more common when mechanical thrombectomy is performed distal to MCA M1 segment [18]. Therefore, accessing a tortuous DMVO using a dedicated suction catheter may be difficult or even risky. The stent retriever is widely used for DMVO; however, it has the disadvantage of the microcatheter being inserted through the occlusion site, which might get damaged during the thrombectomy if the blood vessel is tortuous [14]. Here, we report suction thrombectomies performed using a microcatheter for DMVO that occurred during mechanical thrombectomy for acute ischemic stroke.
All procedures were performed under local anesthesia. No heparin loading was performed, except for a heparinized saline flush. On detecting DMVO on the control angiogram performed during the procedure, a microcatheter (Excelsior XT-27, Stryker, Fremont, CA, USA; Marksman, Medtronic, Irvine, CA, USA) with a microwire (Synchro-14, Stryker, Fremont, CA, USA) was inserted into the guiding catheter. While the microcatheter approached the thrombus, we ensured that the thrombus was untouched by the microwire, and manual aspiration was performed with a 50 ml syringe. When aspirating the blood, we slowly pushed the microcatheter toward the thrombus. Suction was maintained all through the procedure, and maximum suction was achieved when blood aspiration stopped. After 1 min, the microcatheter was removed while suctioning with a 50 ml syringe through a guiding catheter. Angiography was performed after checking the tip, inside the microcatheter, and inside the syringe.
An 81-year-old woman was admitted complaining of drowsiness and left-sided weakness. The patient had atrial fibrillation and was treated with aspirin. The initial National Institutes of Health Stroke Scale (NIHSS) score was 15. Magnetic resonance angiography (MRA) revealed right MCA M1 occlusion. Intravenous tissue plasminogen activator (IV-tPA) was administered, and femoral artery puncture was performed within 3 h of onset. The initial angiogram revealed simultaneous right M1 and distal anterior cerebral artery (ACA) occlusions. The right MCA M1 occlusion was successfully recanalized by suction thrombectomy using a 5MAX (Penumbra, Alameda, CA, USA) suction catheter. For right distal ACA segment occlusion, an Excelsior XT-27 microcatheter was delivered with a Synchro-14 microwire just proximal to the thrombus and manual suction using a 50 ml syringe was performed as previously described. After the withdrawal of the microcatheter, a thrombus was found at the microcatheter tip. Follow-up angiography revealed complete recanalization of the ACA. The NIHSS score at discharge after rehabilitation was 6 (Table 1, Fig. 1).
A 67-year-old man presented to the emergency department with right hemiplegia. He was diagnosed with an acute infarction in the left MCA territory caused by atrial fibrillation one year prior and was prescribed a non-vitamin K oral anticoagulant. He had an NIHSS score of 5 with aphasia but was able to live independently. The initial NIHSS score was 13 points. MRI and MRA showed a left posterior inferior cerebellar artery (PICA) territory ischemic signal change with left vertebrobasilar occlusion. On the initial left vertebral artery (VA) angiogram, the left VA V4 segment was not visualized because of distal VA occlusion. On follow-up, left VA angiography after suction thrombectomy using an intermediate catheter (Navien, Medtronic, Irvine, CA, USA) on the distal left VA, the PICA was completely recanalized. However, left distal posterior cerebral artery (PCA) occlusion was noted, which was intact on the right VA angiogram. A Marksman microcatheter was placed at the occlusion site using a Synchro-14 wire. After suction with a 50 ml syringe and withdrawal of the microcatheter, a thrombus was noted at the microcatheter tip. A follow-up angiogram showed partial recanalization of the left distal PCA with relatively good leptomeningeal collaterals. The operator decided to stop the procedure, and a minimal new lesion was noted on post-thrombectomy diffusion-weighted imaging (DWI) in the left PCA territory. The patient was discharged and was able to walk independently on postoperative day 7 (Table 1, Fig. 2).
An 86-year-old male patient was transferred from another hospital with decreased consciousness, left-sided weakness, and dysarthria. Occlusion of the top of the basilar artery (BA) was noted on MRA with restriction of diffusion in the right pons, midline of the midbrain, and left thalamus. The initial NIHSS score was 14 points. IV-tPA was started before mechanical thrombectomy. Right PCA and left superior cerebellar artery (SCA) distal occlusions were noted on the initial angiogram, while the BA top occlusion was recanalized. After introducing the Marksman microcatheter into the right distal PCA occlusion, suction thrombectomy was successfully performed. However, it was not possible to insert the same microcatheter into the left SCA because of acute angulation. A Prowler Select Plus microcatheter (Cerenovus, Irvine, CA, USA) was introduced, and recanalization was accomplished with stent retriever thrombectomy. Contrast-enhanced MRA performed 24 h later confirmed successful recanalization. The NIHSS score at discharge was 1 (Table 1, Fig. 3).
Mechanical thrombectomy using a stent retriever or suction catheter has been reported to improve longterm outcomes in patients with acute large vessel occlusions [1,2,7,12,20]. Recent reports have claimed the safety and feasibility of mechanical thrombectomy for DMVO [11,16,21,22]. Most studies treated DMVO using stent retrievers and dedicated suction catheters, such as 3MAX and 4MAX, but very few studies treated DMVO with suction thrombectomy using a microcatheter [3,4,13]. In our report, suction thrombectomy using a microcatheter was performed in three cases of DMVO that occurred during mechanical thrombectomy, and successful results were obtained.
The stent retriever not only been reported to have good results in DMVO but also to have a higher first pass rate and lower probability of combining with adjuvant therapy compared to the 3MAX suction catheter [10,11]. However, there was no difference in clinical outcomes, and although the difference was not statistically significant, hemorrhagic complications were higher in the stent retriever thrombectomy group [10]. Wedge problems and vessel injuries are more likely to occur when a stent retriever is used in DMVO [14]. In stent retriever thrombectomy, accessing the distal vessel necessitating passage only through a microcatheter, may be easier than suction thrombectomy, which requires access to a relatively large, dedicated catheter. But a stent retriever tended to cause more vessel injury during thrombectomy. Economically, suction thrombectomy using only a microcatheter and a 50 ml syringe may be better than stent retriever thrombectomy [8].
The contact area and intensity of the negative pressure are the two most crucial factors when extracting a thrombus with suction [5,8]. Although the cross-sectional area of the microcatheter tip is very small compared to that of the dedicated suction catheter, the ratio of the areas between the microcatheter tip and the vessel lumen is not low considering the small diameter of the distal small artery too. Hence, we can expect a sufficient contact interface between the microcatheter tip and thrombus. Sufficient suction power of the microcatheter with only a 50 ml manual syringe can also be verified, considering that the thrombus was partially sucked and tightly attached to the microcatheter tip in all cases (Figs 1, 2, 3).
Gunning et al. have reported that cardio-embolic thrombi are rigid and often slip during stent retriever thrombectomy [9]. Therefore, Qiu et al. suggested that suction thrombectomy may be more appropriate for cardio-embolic thrombi [17]. Since all our cases occurred due to cardioembolism, and we were able to successfully perform suction thrombectomy using a microcatheter their suggestion can be considered reasonable.
Suction thrombectomy using a microcatheter has also been reported in cases of DMVO that occurred during stent angioplasty for M1 stenosis and coil embolization [4,13]. Crockett et al. performed a suction thrombectomy for DMVO using a microcatheter and reported good results of 100% modified Treatment in Cerebral Ischemia (mTICI) 2C/3 without complications [3]. We believe that suction thrombectomy using a microcatheter can be a suitable alternative for DMVO that is too tortuous, increasing risk of vessel injury during stent retriever thrombectomy, or making dedicated suction catheter access difficult.
Based on our experience, suction thrombectomy with a microcatheter through manual aspiration using a 50 ml syringe can be a feasible and effective treatment option for DMVO. We anticipate that this technique may show similar effectiveness in reducing the risk of vessel injury as stent retriever thrombectomy, in patients with tortuous DMVO.
Fig. 1.
Case 1. (A) Initial angiogram showing concurrent middle cerebral artery and distal anterior cerebral artery (arrow) occlusions. (B) After intra-arterial thrombectomy for M1 occlusion with Penumbra 5Max, distal anterior cerebral artery occlusion remained (arrow). (C) Angiogram following suction thrombectomy for distal anterior cerebral artery occlusion with Excelsior XT-27 microcatheter (Stryker, USA) showing near complete recanalization of previous occlusions. (D) Photograph of the tip of Excelsior XT-27 microcatheter which is attached to the thrombus. Note that the very distal part of the microcatheter lumen is filled by thrombus (arrow).
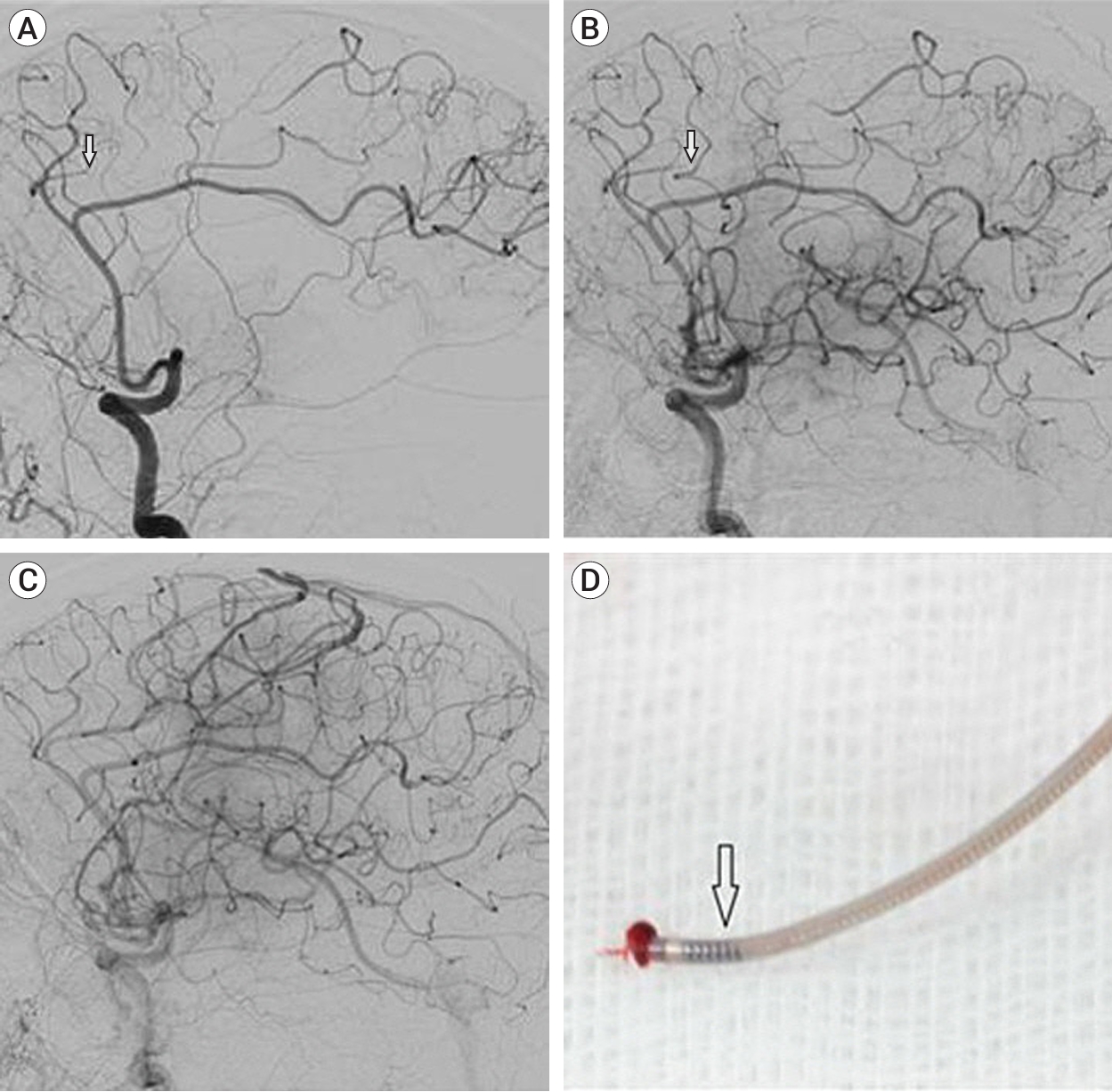
Fig. 2.
Case 2. (A) Initial right vertebral artery angiography showing intact distal arteries while no visualization of distal left vertebral artery is noted (arrow). (B) Left distal posterior cerebral artery occlusion (arrow) is noted on follow-up left vertebral artery angiogram after suction thrombectomy to distal left vertebral artery. Previously occluded left posterior inferior cerebellar artery is now intact after thrombectomy. (C) Forward movement of the Marksman microcatheter (Medtronic, USA) tip (arrow) is noted at the end of the distal posterior cerebral artery thrombectomy using Marksman microcatheter. (D) Photograph of the tip of the Marksman microcatheter with an attached thrombus. Note that the very distal part of the microcatheter lumen is filled by thrombus (arrow).

Fig. 3.
Case 3. (A) Initial angiogram showing concurrent right distal posterior cerebral artery (complete, arrow) and left superior cerebellar artery (incomplete, star) occlusions. (B) Roadmap image showing Marksman microcatheter (Medtronic, USA) (arrow) approaching the thrombus for distal posterior cerebral artery occlusion inside the intermediate catheter (star). (C) Angiogram after microcatheter suction showing complete recanalization of the right posterior cerebral artery. Left superior cerebellar artery occlusion was recanalized with Solitaire Prime with Prowler Select plus microcatheter thereafter. Acute angulation of left superior cerebellar artery hindered approaching of the Marksman microcatheter to the distal occlusion site. (D) Photograph of the tip of the Marksman microcatheter with the thrombus attached. Note that the very distal part of the microcatheter lumen is filled by thrombus (arrow)
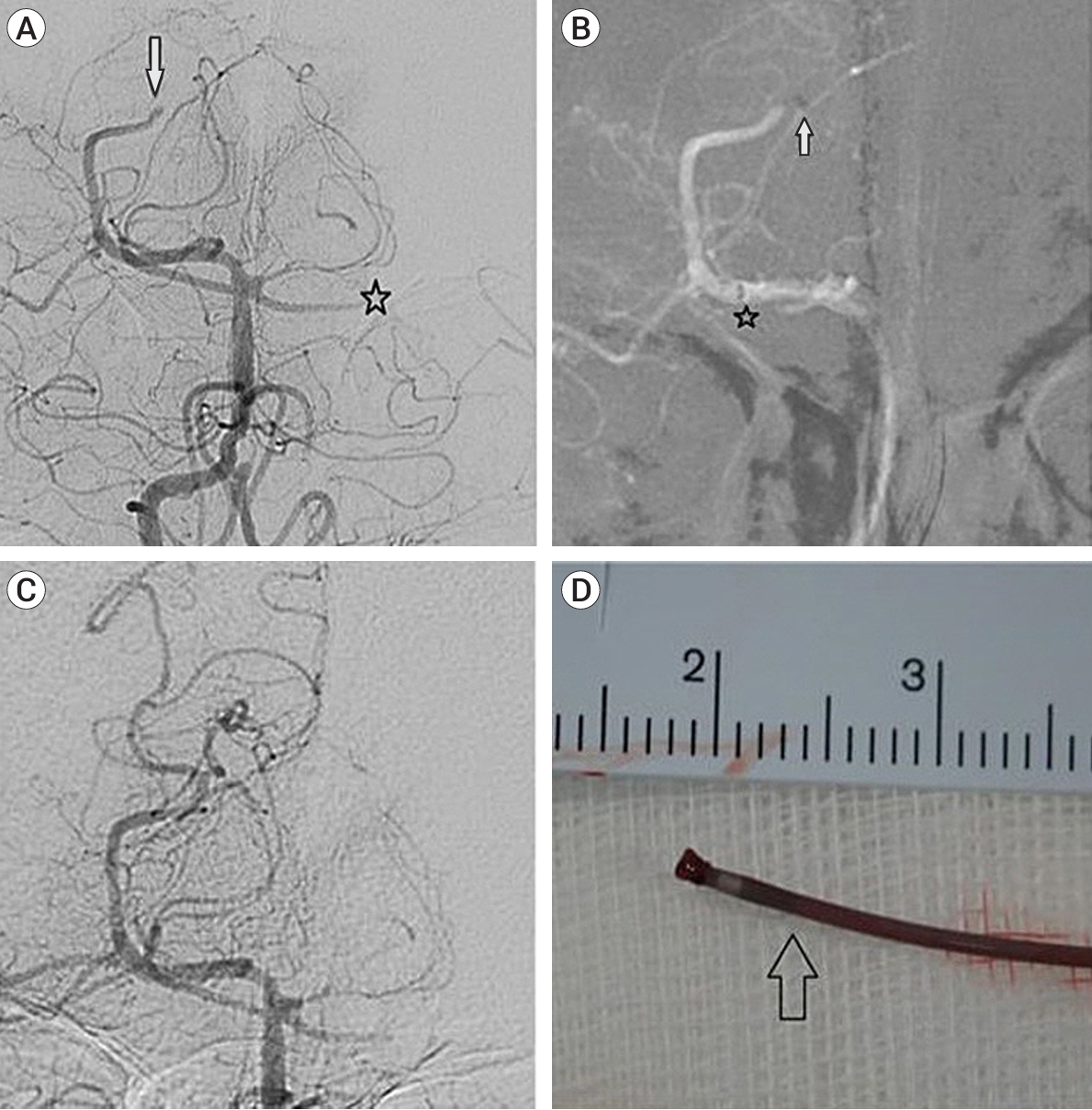
Table 1.
Clinical and radiological findings of the 3 patients undergoing suction thrombectomy using microcatheter
REFERENCES
1. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015 Jan;372(1):11-20.

2. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015 Mar;372(11):1009-18.

3. Crockett MT, Phillips TJ, Chiu AHY. Dual suction Headway27 microcatheter thrombectomy for the treatment of distal intracranial arterial occlusion strokes: Initial experience with the micro-ADAPT technique. J Neurointerv Surg. 2019 11(7):714-8.


4. Drakopoulou M, Giannopoulou A, Zampakis P, Messinis L, Theofanopoulos A, Constantoyannis C, et al. Suction thrombectomy using a microcatheter as a salvage method for acute distal occlusion during cerebral aneurysm embolization: A case report. Brain Circ. 2022 Jun;8(2):112-6.



5. Froehler MT. Comparison of vacuum pressures and forces generated by different catheters and pumps for aspiration thrombectomy in acute ischemic stroke. Interv Neurol. 2017 Oct;6(3-4):199-206.




6. Gory B, Lapergue B, Blanc R, Labreuche J, Ben Machaa M, Duhamel A, et al. Contact aspiration versus stent retriever in patients with acute ischemic stroke with M2 occlusion in the ASTER randomized trial (contact aspiration versus stent retriever for successful revascularization). Stroke. 2018 Feb;49(2):461-4.


7. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015 Mar;372(11):1019-30.

8. Gross BA, Jadhav AP, Jovin TG, Jankowitz BT. Dump the pump: Manual aspiration thrombectomy (MAT) with a syringe is technically effective, expeditious, and cost-efficient. J Neurointerv Surg. 2018 Apr;10(4):354-7.


9. Gunning GM, McArdle K, Mirza M, Duffy S, Gilvarry M, Bouwer PA. Clot friction variation with fibrin content; implications for resistance to thrombectomy. J Neurointerv Surg. 2018 Jan;10(1):34-8.


10. Haussen DC, Eby B, Al-Bayati AR, Grossberg JA, Rodrigues GM, Frankel MR, et al. A comparative analysis of 3MAX aspiration versus 3 mm Trevo Retriever for distal occlusion thrombectomy in acute stroke. J Neurointerv Surg. 2020 Mar;12(3):279-82.


11. Haussen DC, Lima A, Nogueira RG. The Trevo XP 3×20 mm retriever (‘Baby Trevo’) for the treatment of distal intracranial occlusions. J Neurointerv Surg. 2016 Mar;8(3):295-9.


12. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015 Jun;372(24):2296-306.


13. Kwon HJ, Shin JW, Park BS, Lim JW, Jeong HS, Song HJ, et al. Use of microcatheters for suction thrombectomy of acute distal occlusions. Neuroradiology. 2018 Dec;60(12):1357-60.



14. Mokin M, Fargen KM, Primiani CT, Ren Z, Dumont TM, Brasiliense LB, et al. Vessel perforation during stent retriever thrombectomy for acute ischemic stroke: Technical details and clinical outcomes. J Neurointerv Surg. 2017 Oct;9(10):922-8.


15. Mokin M, Primiani CT, Ren Z, Kan P, Duckworth E, Turner RD 4th, et al. Endovascular treatment of middle cerebral artery M2 occlusion strokes: Clinical and procedural predictors of outcomes. Neurosurgery. 2017 Nov;81(5):795-802.


16. Navia P, Larrea JA, Pardo E, Arce A, Martínez-Zabaleta M, Díez-González N, et al. Initial experience using the 3MAX cerebral reperfusion catheter in the endovascular treatment of acute ischemic stroke of distal arteries. J Neurointerv Surg. 2016 Aug;8(8):787-90.


17. Qiu K, Zhao LB, Xu XQ, Wang Y, Liu J, Liu S, et al. Acute embolic stroke with large-vessel occlusion: Does contact aspiration thrombectomy show superiority? Clin Radiol. 2022 Aug;77(8):577-83.


18. Saber H, Narayanan S, Palla M, Saver JL, Nogueira RG, Yoo AJ, et al. Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: A meta-analysis. J Neurointerv Surg. 2018 Jul;10(7):620-4.


19. Sarraj A, Sangha N, Hussain MS, Wisco D, Vora N, Elijovich L, et al. Endovascular therapy for acute ischemic stroke with occlusion of the middle cerebral artery M2 segment. JAMA Neurol. 2016 Nov;73(11):1291-6.


20. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015 Jun;372(24):2285-95.


-
METRICS

-
- 0 Crossref
- 0 Scopus
- 351 View
- 29 Download
- ORCID iDs
-
Hyeon-Song Koh

https://orcid.org/0000-0003-2659-5535 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



