 |
 |
| J Cerebrovasc Endovasc Neurosurg > Epub ahead of print |
Abstract
Cranial nerve palsies can be presenting signs of intracranial aneurysms. There is a classic pairing between an aneurysmal vessel and adjacent nerves leading to cranial neuropathy. Isolated abducens nerve palsy can be a localizing sign of an unruptured vertebrobasilar circulation aneurysm. Aneurysms involving Anterior Inferior Cerebellar Artery (AICA) and Posterior Inferior Cerebellar Artery (PICA) have been reported to be associated with abducens nerve palsy. The symptoms in unruptured aneurysms are due to the mass effect on adjacent neurovascular structures. Most of the abducens nerve palsy resolves following microsurgical clipping. Here, we present a rare case of an unruptured Posterior Cerebral Artery (PCA) aneurysm presenting with abducens nerve palsy and diplopia associated with contralateral hemianopsia which markedly improved following endovascular coil embolization.
Cranial nerve palsies can be presenting signs of intracranial aneurysms. There is a classic pairing between an aneurysmal vessel and adjacent nerves leading to cranial neuropathy. In unruptured aneurysms, it is due to their mass effect on the adjacent nerve. However, in case of a ruptured aneurysm, it is due to raised intracranial pressure, direct irritation, or stretching of the nerve by blood in the subarachnoid space. Aneurysms involving Anterior Inferior Cerebellar Artery (AICA) and Posterior Inferior Cerebellar Artery (PICA) have been reported to be associated with abducens nerve palsy [5,11]. Aneurysm of the posterior cerebral artery (PCA) is uncommon accounting for 1% of all intracranial aneurysms [1,9]. Unruptured giant aneurysms possess a substantial risk of rupture but are frequently asymptomatic [12]. Those with symptoms have headaches of vascular type with no neurological deficits. They may also manifest with loss of visual acuity and cranial nerve deficits.
We report the rare case of an unruptured left P1 PCA segment saccular aneurysm first presenting with abducens nerve palsy and diplopia which markedly improved following endovascular coil embolization. This is the first case of an isolated abducens nerve palsy associated with an unruptured PCA aneurysm.
A 37-year-old female presented to a local hospital with an acute onset holo cranial headache associated with vomiting. It was followed by a brief loss of consciousness. She was managed conservatively with some relief of symptoms. She later developed symptoms of diplopia with decreased vision on the right temporal side. Past medical history was unremarkable. She denied any past similar episodes, seizures, or motor and sensory deficits.
On examination, her initial vital signs were essentially normal. Her general physical examination was normal. However, on neurological examination, she demonstrated a left sixth cranial nerve (CN) palsy (left abductor paresis) with right homonymous hemianopsia. The remaining cranial nerves, strength, sensation, and gait were tested and found to be intact.
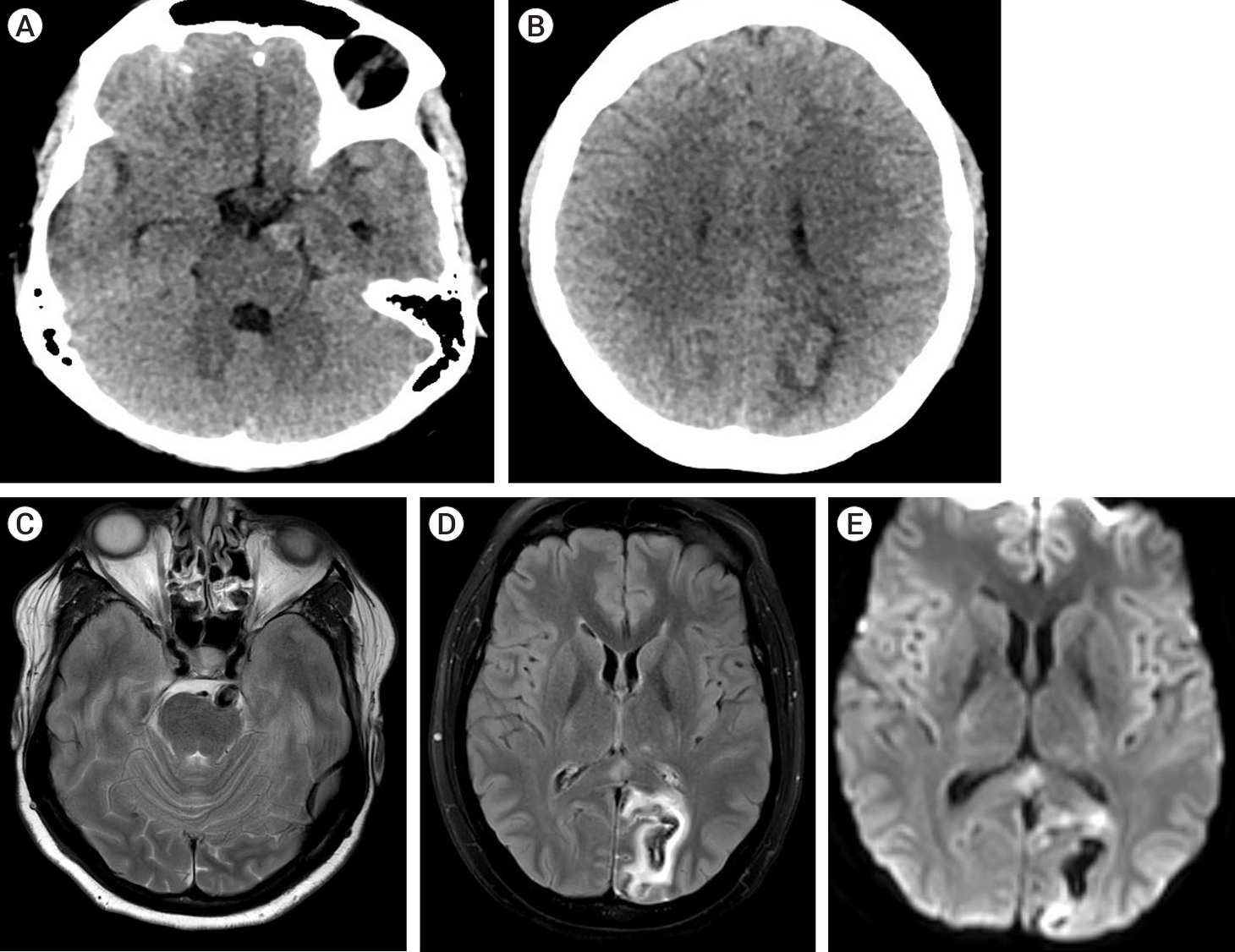
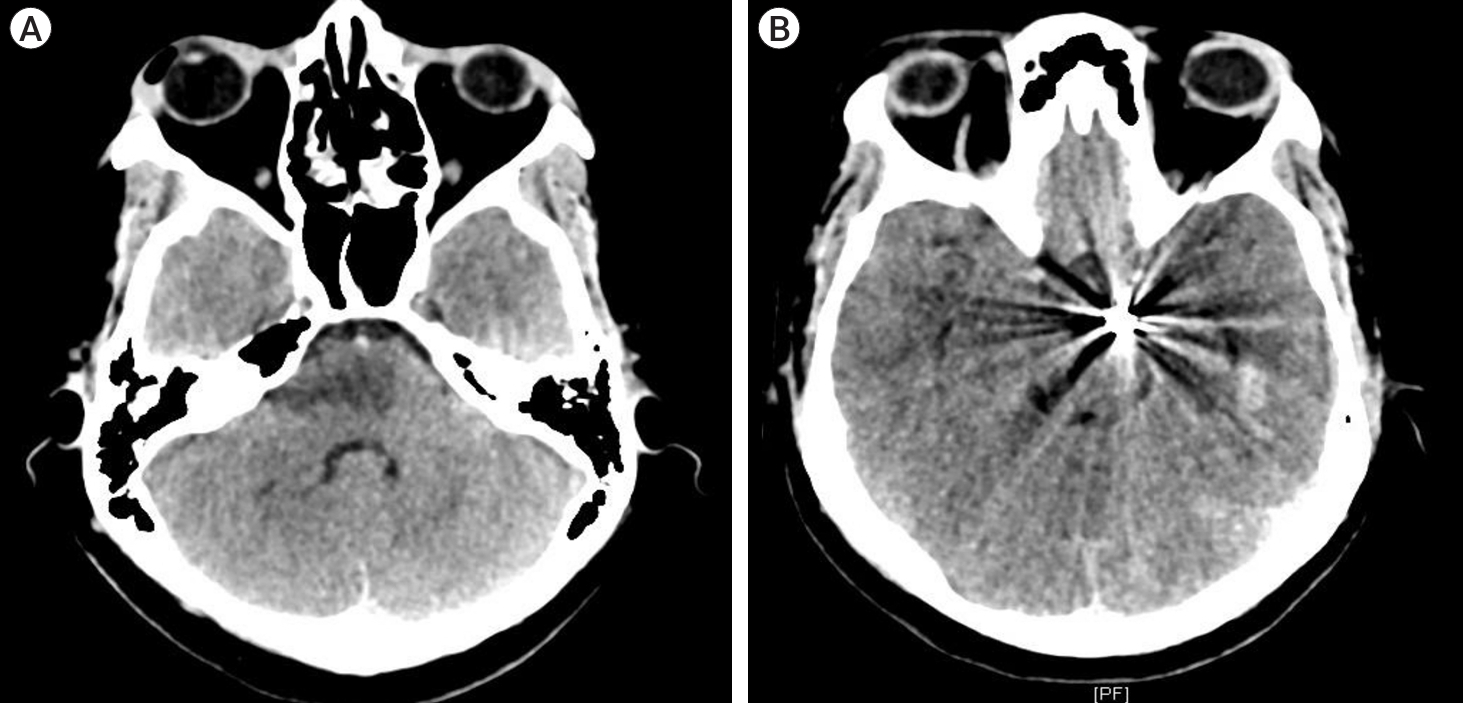
Blood investigations were essentially normal. Based on her clinical manifestations, a non-enhanced CT scan was obtained which showed a left PCA territory infarct (Fig. 1A, B). Subsequent magnetic resonance imaging (MRI) demonstrated areas of subacute infarct in the left PCA territory and a partially thrombosed dissecting fusiform aneurysm involving the left proximal P2 PCA (Fig. 1C, D, E). Angiography revealed a large dissecting fusiform aneurysm measuring 7.51 mm×8.75 mm×7.99 mm involving the P1-P2 PCA with good cross flow across the left posterior communicating artery (PCOM) (Fig. 2A, B).
The patient underwent successful endovascular coiling of the left P1-P2 PCA aneurysm with parent artery occlusion with multiple detachable coils. Post-coiling angiogram showed complete occlusion of the aneurysm and the left PCA (Fig. 2C, D).
The immediate postoperative period was unremarkable except for mild left hemiparesis. She had relief of headache but no significant improvement of left lateral rectus palsy was noted on the first postoperative day. She demonstrated improvement of lateral movement in the left eye on the third postoperative day, which resolved completely at discharge. Her hemiparesis improved during subsequent follow-up visits.
PCA aneurysms are different from their counterparts by their characteristic morphologic features and clinical manifestations. They tend to appear at an earlier age, with an average age of 38 years (10-20 years earlier than other intracranial aneurysms) [1,6,9]. These aneurysms are more frequently giant and dissecting in comparison to aneurysms of other anatomic sites [1,2,9]. The dissection typically occurs between intima and media of PCA [8]. Dissecting PCA aneurysms tend to occur in normotensive female patients often presenting with occipital headache [4,8,10]. They can also present with symptoms of mass effect on adjacent brain parenchyma [1,3,6]. The most common clinical presentation of ruptured aneurysms is subarachnoid hemorrhage (SAH) (severe headache) followed by ischemia or infarction [10]. The patients harboring PCA aneurysms have visual disturbances like oculomotor palsy and homonymous hemianopsia. Giant aneurysms of the P1 segment can also compress the optic chiasm and cause bitemporal hemianopsia [1].
CN III has been associated with PCA aneurysms. CN VI palsy has been associated with PICA, AICA, and cavernous ICA aneurysms. However, this case illustrates a PCA aneurysm causing ipsilateral CN VI palsy and contralateral hemianopsia which is a rare phenomenon. The left CN VI palsy can be attributed to the aneurysm causing a mass effect on adjacent ventral left hemipons. The right homonymous hemianopsia can be explained by the left PCA territory infarct likely due to emboli from the aneurysm or direct mass effect on the PCA itself. Therefore, the symptoms complex of PCA aneurysms depends on the segment involved. In general, giant aneurysms involving the P1 and P2 segments present with visual disturbances (CN III palsy and homonymous hemianopsia), and the P3 segment with sleepiness and memory loss (compression on brainstem and hippocampus respectively) [1]. The left hemiparesis post endovascular coiling could be due to temporary increase in the volume of the aneurysm, due to coil and thrombus formation, resulting in edema (Fig. 3).
Microsurgery and endovascular therapy are the available modalities to occlude these aneurysms. Most of the abducens nerve palsy resolves following microsurgical clipping. However, these procedures are complex due to the deep anatomical location of these aneurysms and their proximity to the brainstem. Therefore, these carry significantly higher morbidity rates [7]. Endovascular therapy with coil embolization is another option that can be performed without any significant risk to the parent artery. The abducens nerve palsy and diplopia improved markedly following endovascular coil embolization in this case.
PCA aneurysms can have a wide array of presentations. The visual disturbances commonly include CN III palsy and homonymous hemianopsia. Isolated abducens palsy has been associated with AICA, PICA, and cavernous ICA aneurysms. These dissecting PCA aneurysms can also rarely present with CN VI palsy and therefore, provide indirect information regarding the aneurysm location and size. It could be regarded as a symptom resulting from the complex neural anatomy of the brain stem, possibly caused by a downward configuration of the PCA aneurysm. This is a maiden case of PCA aneurysm presenting with abducens palsy which was successfully resolved with coil embolization.
Fig. 1.
(A, B) Non-enhanced CT Scan Head showing a hyperdense lesion in the left crural cistern. Left PCA territory infarct without SAH. (C, D, E) Areas of subacute infarct in left PCA territory involving left cuneus and posterior cingulate cortex with hemorrhagic transformation and cortical laminar necrosis involving left cuneus, likely emboli from aneurysm. Partially thrombosed dissecting fusiform aneurysm involving left proximal P2 PCA, with mild mass effect and edema involving adjacent ventral left hemipons. CT, computed tomography; PCA, posterior cerebral artery; SAH, subarachnoid hemorrhage
REFERENCES
1. Ciceri EF, Klucznik RP, Grossman RG, Rose JE, Mawad ME. Aneurysms of the posterior cerebral artery: Classification and endovascular treatment. AJNR Am J Neuroradiol. 2001 Jan;22(1):27-34.


2. Drake CG, Peerless SJ, Hernesniemi JA. Surgery of Vertebrobasilar Aneurysms: London, Ontario Experience on 1767 Patients. Vienna: Springer Vienna; 1996.
3. Gerber CJ, Neil-Dwyer G. A review of the management of 15 cases of aneurysms of the posterior cerebral artery. Br J Neurosurg. 1992 6(6):521-7.


4. Oran I, Cinar C, Yağci B, Tarhan S, Kiroğlu Y, Serter S. Ruptured dissecting aneurysms arising from non-vertebral arteries of the posterior circulation: Endovascular treatment perspective. Diagn Interv Radiol. 2009 Sep;15(3):159-65.

5. Parr M, Carminucci A, Al-Mufti F, Roychowdhury S, Gupta G. Isolated abducens nerve palsy associated with ruptured posterior inferior cerebellar artery aneurysm: Rare neurologic finding. World Neurosurg. 2019 Jan;121:97-9.


6. Pia HW, Fontana H. Aneurysms of the posterior cerebral artery. Locations and clinical pictures. Acta Neurochir (Wien). 1977 38(1-2):13-35.


7. Seoane ER, Tedeschi H, de Oliveira E, Siqueira MG, Calderón GA, Rhoton AL Jr. Management strategies for posterior cerebral artery aneurysms: A proposed new surgical classification. Acta Neurochir (Wien). 1997 139(4):325-31.



8. Sherman P, Oka M, Aldrich E, Jordan L, Gailloud P. Isolated posterior cerebral artery dissection: Report of three cases. AJNR Am J Neuroradiol. 2006 Mar;27(3):648-52.



9. Suzuki O, Miyachi S, Negoro M, Okamoto T, Sahara Y, Hattori K, et al. Treatment strategy for aneurysms of the posterior cerebral artery. Interv Neuroradiol. 2003 May;9(Suppl 1):83-8.


10. Taqi MA, Lazzaro MA, Pandya DJ, Badruddin A, Zaidat OO. Dissecting aneurysms of posterior cerebral artery: Clinical presentation, angiographic findings, treatment, and outcome. Front Neurol. 2011 Jun;2:38.



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 409 View
- 10 Download
- ORCID iDs
-
Sabina Regmi

https://orcid.org/0000-0002-9827-8320 - Related articles




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



